

Just Diagnosed? 9 Questions about Pituitary Tumors Answered
by Zara Jethani
Being diagnosed with a pituitary tumor or adenoma can feel overwhelming. Patients often have questions that aren’t always fully covered during an initial appointment. To help you better understand what to expect, Garni Barkhoudarian, MD, expert neurosurgeon and co-director of the Pacific Pituitary Disorders Center, shares answers to the most common concerns people have after a diagnosis.
For a detailed clinical overview of pituitary adenomas, visit our Pituitary Adenomas Conditions page.
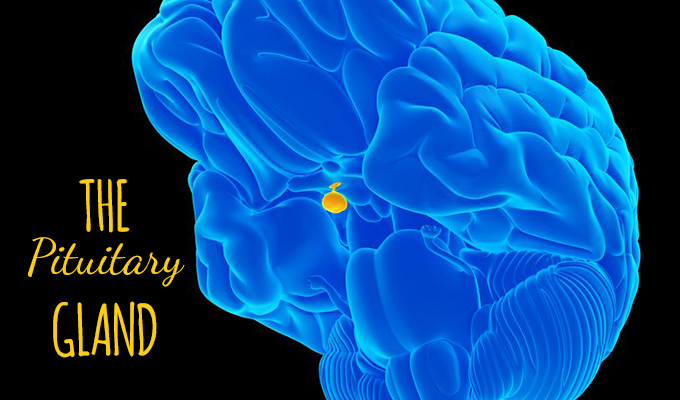
What symptoms should I expect with a pituitary tumor?

When there is a tumor on the pituitary gland, symptoms may vary depending on the particular diagnosis. The most common symptoms are headaches, vision loss or double vision, and hormone dysfunction which can include fatigue, weight gain, loss of menstrual cycle and impotence. In some cases, pituitary tumors can be truly asymptomatic.
Knowing these symptoms can help you track changes and better communicate with your healthcare team.
What’s the difference between a pituitary tumor, lesion, and a pituitary tumor?
A pituitary tumor is considered a type of brain tumor. Pituitary lesions may also include cysts and inflammatory conditions that may mimic tumors.
Your doctor may use these terms interchangeably, which can be confusing. Don’t hesitate to ask for clarification on what exactly your diagnosis means.
What are my treatment options after a pituitary tumor diagnosis?

One specific type of pituitary tumor, a prolactinoma (pituitary adenoma that secretes the hormone prolactin), can be very successfully treated with medications (cabergoline or other dopamine agonist).
In all other patients who have symptomatic pituitary adenomas or have a growing tumor, especially in patients with Cushing’s disease or acromegaly, or other pituitary conditions such as central hyperthyroidism, craniopharyngioma and chordoma, surgical resection is best.
We recommend an endoscopic endonasal surgical removal of the tumor by an experienced team, ideally consisting of both a neurosurgeon and ENT surgeon.
Treatment is personalized based on the tumor type, hormone involvement, and symptoms. Your doctor will guide you through the most effective approach.
How risky is pituitary tumor surgery?
There are always risks with any surgery. Though not very common, there are certainly serious complications that can occur during or after pituitary tumor surgery. These range from sinus infection, bleeding and hormone dysfunction to meningitis, vision loss, stroke and even death. Thankfully, the risks of these major complications are low (1-3%).
While the risks are real, experienced neurosurgical teams like ours maintain a strong safety record and prioritize complication avoidance.
How long does pituitary tumor surgery take and what’s recovery like?
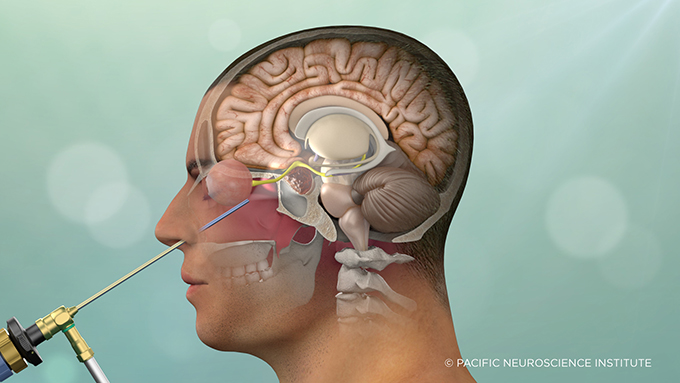
The duration of pituitary tumor surgery varies based on the tumor type, specific location, invasiveness and goals of surgery. The typical operation is around 3 hours, but can be upwards of 8-10 hours for rare tumors.
Most patients stay in the hospital for 1–2 days. Recovery typically includes hormone monitoring, vision checks, and follow-up imaging.
Are pituitary tumors common?

Pituitary tumors and cysts are very common, being identified in about one in six people. However, those that need surgery are much less common, affecting approximately 1/10,000 people annually.
Just because a pituitary tumor is detected doesn’t always mean it requires immediate treatment—many are monitored over time.
Will my tumor grow—and how fast?
Most pituitary tumors are slow growing, approximately 1-3mm/year.
Your care team will likely use MRI scans to monitor tumor size and determine if and when treatment is needed.
Is there a chance the tumor could return?
This depends on the tumor type and pathological features. Most pituitary tumors have a recurrence rate of about 10% over 10 years. Craniopharyngiomas, chordomas and Cushing’s disease tend to have faster recurrence rates.
Regular follow-ups after treatment are important to detect recurrence early.
Where can I find support and education resources?
Yes, some resources for education and community support include:
- Pituitary Network Association
- pituitarysociety.org/patient-education
- cushings-help.com
- hormones411.org
These organizations provide support groups, educational content, and patient stories. You are not alone.
Ready to Talk to a Specialist?
If you’ve been recently diagnosed with a pituitary adenoma, it’s important to meet with a team experienced in treating these conditions. At Pacific Neuroscience Institute, our specialists provide expert diagnosis, personalized care, and advanced minimally invasive treatment options.Schedule a consultation with our Pituitary Disorders team at 310-582-7450 or contact us online.
About Dr. Garni Barkhoudarian
Garni Barkhoudarian, MD, FAANS, is a board-certified, fellowship-trained neurosurgeon with a focus on skull base and minimally invasive endoscopic surgery. Dr. Barkhoudarian has particular interest and expertise in pituitary and parasellar tumors, brain tumors, skull-base tumors (including meningiomas, craniopharyngiomas, chordomas and schwannomas), intra-ventricular brain tumors, colloid cysts, trigeminal neuralgia, hemifacial spasm and other vascular compression syndromes.
Clinic Locations
PNI-SANTA MONICA (map)
PROVIDENCE SAINT JOHN’S HEALTH CENTER
2125 Arizona Ave, Santa Monica, CA 90404
310-829-8319
PNI-SOUTH BAY (map)
PROVIDENCE LITTLE COMPANY OF MARY TORRANCE
5215 Torrance Blvd #300, Torrance, CA 90503
424-212-5361
PNI-BURBANK (map)
PROVIDENCE SAINT JOSEPH MEDICAL CENTER
501 South Buena Vista St, Burbank, CA 91505
818-847-6049 | Fax: 818-847-4842
Useful links
About the Author

Zara Jethani
Zara is the marketing director at Pacific Neuroscience Institute. Her background is in molecular genetics research and healthcare marketing. In addition, she is a graphic designer with more than 20 years experience in the healthcare, education and entertainment industries.
Last updated: May 19th, 2025