Minimally Invasive Brain Tumor Surgery / Keyhole Surgery
What is minimally invasive brain tumor surgery?
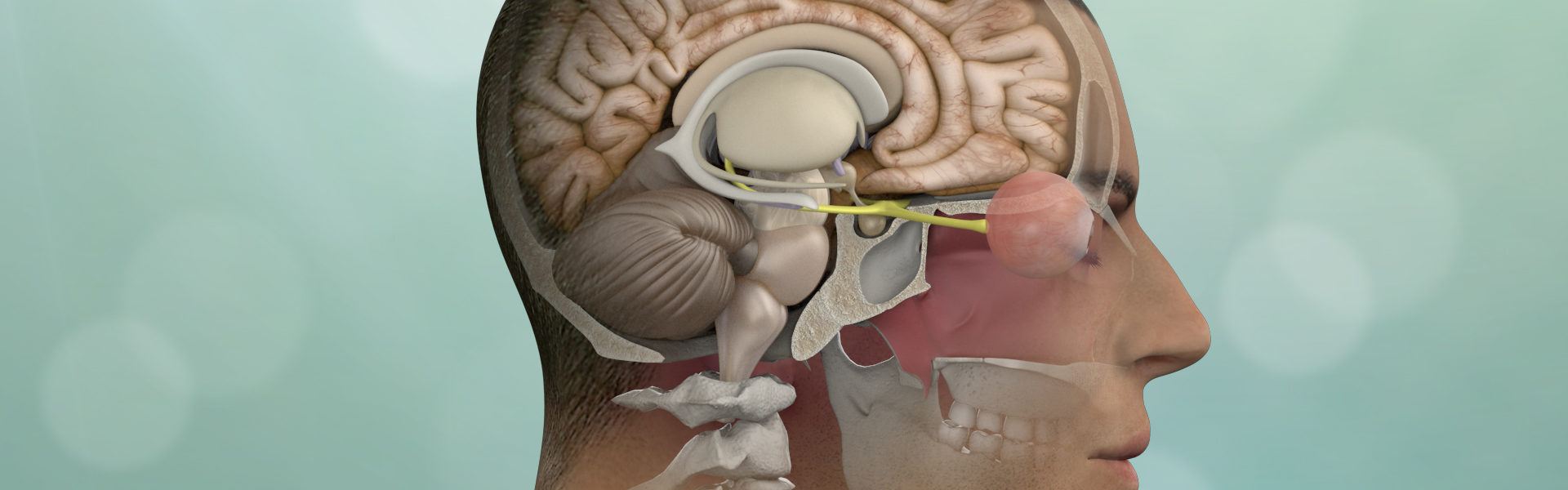
Minimally invasive brain tumor surgery, also known as keyhole surgery or neuroendoscopic surgery, is a surgical approach aimed at removing brain tumors with less disruption to surrounding healthy brain tissue compared to traditional open surgery. It involves the use of specialized instruments and techniques to access and remove the tumor through small incisions or natural body openings, such as the nostrils or mouth.
What is a keyhole operation for brain tumors?
Keyhole surgery is the concept of safely removing brain and skull base tumors through smaller, more precise openings that minimize collateral damage to the surrounding scalp, brain, blood vessels, and nerves.
Fortunately, given advances over the last two decades in technology and instrumentation, as well as, improved brain and skull base anatomical understanding, a majority of brain and skull base tumors can now be removed via one of these approaches using a small craniotomy (bony skull opening) or an approach through the nostrils.
Is keyhole surgery right for you?
While minimally invasive brain tumor surgery offers several potential advantages, it may not be suitable for all types and sizes of brain tumors. Complex or large tumors may still require open surgery for optimal resection and access. Additionally, the decision to pursue minimally invasive surgery versus open surgery is based on careful consideration of individual patient factors, tumor characteristics, and the surgeon’s judgment.
Potential advantages of keyhole brain & skull base tumor removal:
- Smaller incisions and bony openings (or no incision is performed through the nostrils – endonasal)
- Less exposure to normal brain structures
- No use of brain retraction with less manipulation of the brain itself
- Less pain and lower need for narcotics
- Rapid recovery, mobilization, and return to normal activities
- Discharge from hospital typically within 1 to 2 days post-surgery
Notably, these approaches are technically demanding, require specialized instrumentation, significant surgical expertise and are not appropriate for all tumors. Consequently, there remains a role for conventional larger craniotomies.
Our approach to minimally invasive keyhole surgery
The ideal surgical approach for each patient is determined by the specific tumor type and location. Regardless of the route chosen, our goals are to maximize tumor removal and minimize manipulation of critical structures. Thereby avoiding complications and patient disfigurement, while promoting a more rapid, complete and less painful recovery.
Highly skilled surgeons with extensive experience for complicated brain tumor procedures
At Pacific Brain Tumor Center, our number one goal is restoring or maintaining our patients’ quality of life. Our team of neurosurgeons and ENT/ skull base surgeons led by Center Director, Dr. Daniel Kelly has been at the global forefront of advancing these minimally invasive approaches for a wide range of common and uncommon brain and skull base tumors including:
Dr. Kelly and his team have extensive expertise with both conventional and keyhole approaches totaling over 4,500 such procedures over the past two decades. This large experience allows us to provide a truly tailored approach best suited for each patient.
Types of Keyhole Brain Tumor Surgery:
- Supraorbital
- endoscopic endonasal
- mini-pterional
- retromastoid
- gravity-assisted
- endoscopic transventricular
- brain port
Supraorbital Eyebrow Craniotomy

When would the supraorbital eyebrow craniotomy procedure be performed?
The supraorbital eyebrow approach is useful for many patients with meningiomas, craniopharyngiomas and other tumors near the optic nerves and pituitary gland, as well as gliomas and metastatic brain tumors in the frontal and temporal lobes.
This versatile, minimally invasive approach minimizes normal tissue disruption and brain retraction, allowing for a more direct approach to these lesions. Occasionally, an abdominal fat graft may be necessary to seal large nasal sinus defects.
This approach is typically performed with the assistance of an endoscope, allowing for further visualization. As such, patients recover well and have good cosmetic outcomes long term.
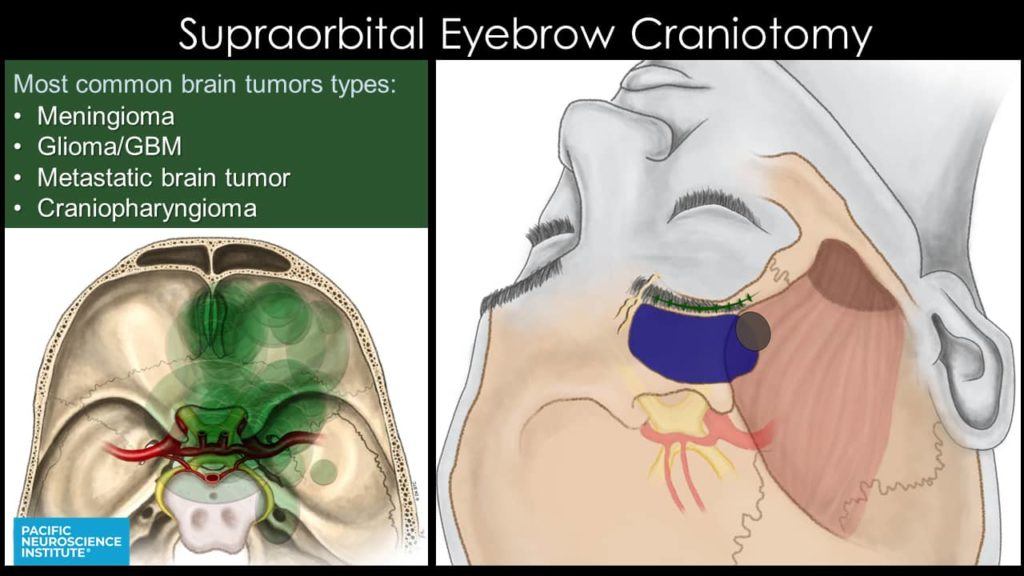
At the Pacific Brain Tumor Center, we have extensive experience with this approach, helping pioneer this operation since its introduction.
We have published extensively on this topic.
Supraorbital Craniotomy vs. MiniPterional Craniotomy
At PNI, for tumors of the frontal or middle fossa, we routinely use the supraorbital or minipterional approaches instead of the traditional larger pterional (fronto-temporal) or bi-frontal craniotomies that involve larger scalp incisions and bony openings. Endoscopy and low-profile instruments allow excellent access to tumors through these smaller keyhole openings.

Endoscopic Endonasal Approach (through the nostrils)
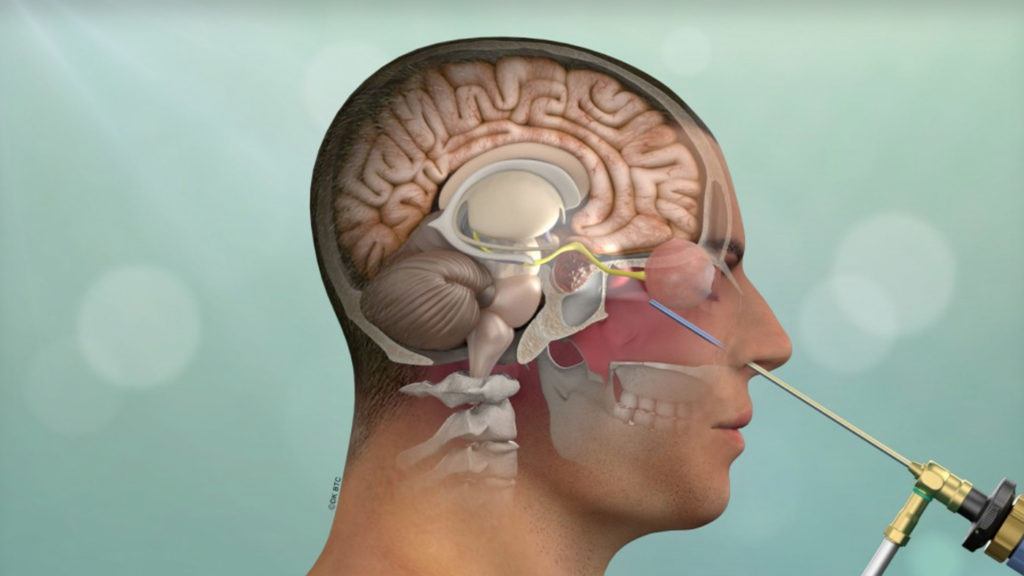
When would the endoscopic endonasal surgery procedure be performed?
Endoscopic Endonasal Surgery (through the nostrils) is ideal for most pituitary adenomas, craniopharyngiomas, chordomas, sinus carcinomas, olfactory neuroblastomas and some midline meningiomas of the tuberculum sellae, clivus, cavernous sinus, Meckel’s cave, orbital apex and orbit.
Endoscopic Endonasal Surgery (through the nostrils) is ideal for most pituitary adenomas, craniopharyngiomas, chordomas, sinus carcinomas, olfactory neuroblastomas and some midline meningiomas of the tuberculum sellae, clivus, cavernous sinus, Meckel’s cave, orbital apex and orbit.
We have published extensively on this topic.
Mini-Pterional Approach
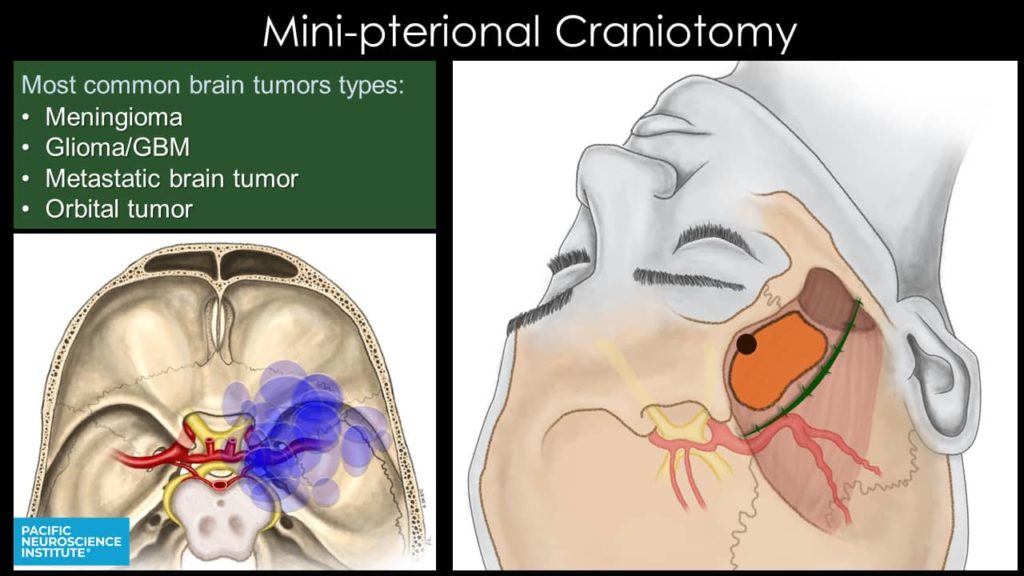
When would the endoscopic mini-pterional craniotomy procedure be performed?
The Mini-Pterional Approach offers a direct avenue for certain sphenoid wing and parasellar meningiomas, other tumors of the cavernous sinus and Meckel’s cave, orbital lesions as well as temporal lobe gliomas and metastatic brain tumors.
Typically, this operation is assisted with endoscopic visualization, allowing for increased visualization of the structures in the region. Patients recover relatively quickly in comparison with traditional pterional operations, with potentially less pain, chewing difficulties and facial muscle atrophy.
Supraorbital Craniotomy vs. MiniPterional Craniotomy
At PNI, for tumors of the frontal or middle fossa, we routinely use the supraorbital or minipterional approaches instead of the traditional larger pterional (fronto-temporal) or bi-frontal craniotomies that involve larger scalp incisions and bony openings. Endoscopy and low-profile instruments allow excellent access to tumors through these smaller keyhole openings.

Retromastoid Craniotomy Approach (behind the ear)

When would the retromastoid craniotomy procedure be performed?
The retromastoid approach (also known as the retrosigmoid approach) uses a small window behind the ear to reach and remove acoustic and trigeminal schwannomas, meningiomas, epidermoid tumors, and tumors of the cerebellum such as hemangioblastomas and metastatic brain tumors.
It is also the main approach for microvascular decompression of the cranial nerves (for trigeminal neuralgia or hemifacial spasm). This operation is augmented with the introduction of the endoscope, allowing for visualization around corners, limiting the need for extensive tissue removal or brain retraction.
Occasionally, an abdominal fat graft is necessary to seal the opening and prevent a cerebrospinal fluid (CSF) leak.
Overall, this operation is associated with great access to the pathology with minimal cosmetic or soft-tissue damage and relatively quick patient recovery.
Gravity-Assisted Brain Tumor Surgery Approaches

Types of Gravity Assisted Brain Tumor Surgery
Trans-Falcine Approach
By using gravity to allow for the normal brain to fall away, there is no need for brain retraction and there is minimal normal brain traversed to reach these midline, deep lesions.
When would the gravity-assisted trans-falcine procedure be performed?
The gravity-assisted Trans-Falcine approach is ideal for the resection of meningiomas, gliomas (astrocytomas, ependymomas, oligodendrogliomas, intraventricular tumors) and metastatic brain tumors. The angled endoscopes allow for excellent visualization and the potential of maximal safe tumor resection.
Compared to traditional approaches, patients have a relatively quicker recovery and the potential of increased preservation of neurological function.
Trans-Tentorial Approach
This approach takes advantage of the normal structures separating the cerebral cortex from the other structures of the hindbrain and brainstem, minimizing the need for brain retraction.
When would the gravity-assisted trans-tentorial procedure be performed?
The gravity-assisted trans-tentorial approach is ideal for patients with certain pineal tumors and cysts, gliomas, metastatic tumors and cerebral cavernous malformations of the inferior-medial posterior temporal and occipital lobes.
The operation is performed in a sitting position to achieve this relaxation. Patients will require a pre-operative cardiac evaluation to ensure safe surgical outcomes. This procedure is performed endoscopically, allowing for improved visualization and a smaller craniotomy.
Compared with other approaches, this has less risk to the occipital lobes (vision processing region) and decreased disruption of normal tissue and brain.
Endoscopic Trans-Ventricular Route
For tumors and cysts within the ventricles: colloid cyts, gliomas, metastatic brain tumors and pineal tumors.
Brain Port Approach

When would the brain port procedure be performed?
The Brain Port approach is used for gliomas, metastatic brain tumors and cerebral cavernous malformations deep within the brain.
Challenging deep-seated brain tumors and blood clots can be reached while minimizing the risk of damaging the surrounding dense and delicate neural structures that control brain and body functions.
Using a tool called BrainPath®, Pacific Brain Tumor Center neurosurgeons can navigate between the natural folds and neural structures in the brain, to minimize collateral damage to the surrounding brain along the path to reach the tumor or blood clot.

