Navigating the Brain & Skull Base Safely & Effectively
How We Strive to Make Brain Surgery Safer & More Effective
Maximizing tumor removal and avoiding complications are two key goals of any surgery. In addition to our accumulated skills and experience, we utilize a variety of techniques and technologies to help achieve these goals. Here are 8 such methods we frequently use depending upon the specifics of a given patient.
Surgical Navigation (“GPS for the brain”)
Prior to surgery, a navigational MRI and/or CT scan is performed that is incorporated into a tracking system in the operating room such that a probe placed on the scalp, skull or brain can be precisely anatomically localized within millimeters. This intra-operative “GPS” methodology is used on all operations to help define the ideal scalp incision, bony opening, critical nerves and blood vessels and the tumor itself.
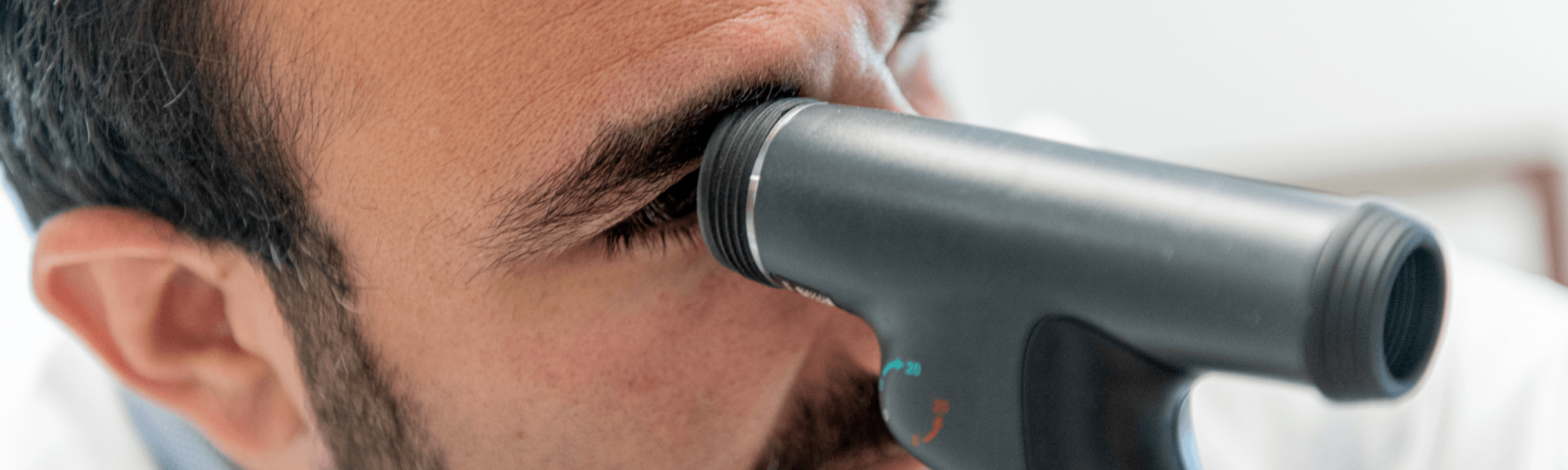
Endoscopy
The panoramic highly detailed view of the high-definition surgical endoscope is in many ways superior to the operating microscope. Thus, it has replaced the microscope as the sole viewing choice for all of our endonasal skull base tumor and pituitary surgeries. The endoscope is also used in most craniotomies to confirm complete or maximal tumor removal and to help with tumor removal itself.
Ultrasound for Tumor Localization
Tumors that are below the brain surface can at times be difficult to find even with surgical navigation due to shifting of the brain after the dura (brain covering) is open. In contrast, an ultrasound probe provides a simple safe real-time image of the brain that can precisely localize deeply situated tumors or those in or under critical brain areas such as the motor cortex. This technique is used most frequently in the removal of certain types of gliomas and metastatic brain tumors.
Ultrasound for Tracking Blood Vessels
Many brain and skull base tumors become intimately attached to critical arteries and veins. Preserving such vessels is essential to avoiding a post-operative stroke. The slender thin Doppler probe provides an accurate real-time method of localizing such vessels that may be hidden directly behind a rind of tumor or dural membrane. The Doppler probe is an essential tool used in every endoscopic endonasal surgery and many craniotomies to avoid vascular injury.
Evoked Potential Monitoring (Neuro-Monitoring)
Removal of many brain and skull base tumors may involve manipulation of fiber tracts, cranial nerves and blood vessels. Neuro-monitoring allows us to electrically track the degree of neural and blood vessel manipulation and serves as an early warning system that a nerve or blood vessel may be overly stressed or damaged. Such neuro-monitoring helps as a means of avoiding neurological complications such as stroke, paralysis and sensory loss.
Awake Craniotomy Technique
In patients with brain tumors within or near critical brain areas such as motor or speech cortex or motor or visual fiber tracts, the patient is awakened during the critical phase of tumor removal. By electrically stimulating the brain areas around the tumor and by interacting with the patient, this neuro-monitoring technique allows a determination of whether it is safe to remove all or only part of the tumor. This technique is used most frequently in the removal of certain types of gliomas and metastatic brain tumors.
Functional MRI & Fiber Tractography
In patients with brain tumors beneath or next to critical brain areas, where critical functions (e.g., motor or language) or critical fiber tracts (e.g., motor or visual tracts) are located, special MRI sequences are performed to determine where these areas or fiber tracts are located. Having this information before surgery, helps select the safest corridor to reach and remove the tumor.
Post-operative Imaging & Monitoring
Careful and frequent surveillance of patients after tumor removal is essential. Patients typically have post-operative imaging (a CT or MRI scan) to assess for any immediate post-operative problems such as bleeding and are carefully monitored in our Saint John’s Intensive Care Unit or Step-Down Unit. Continuous EEG is rarely needed but is available for patients who might be having ongoing seizures. Our comprehensive team includes neurosurgeons, neurologists, hospitalists, critical care specialists, neurosurgical nurse practitioner and ICU nursing staff.
