Craniopharyngioma
On this page: Overview | Symptoms | Diagnosis | Treatment | Doctors and Specialists
What is Craniopharyngioma?
Craniopharyngioma is a rare type of benign brain tumor that develops near the pituitary gland at the base of the brain. This tumor originates from remnants of embryonic tissue that are normally present during early development. Despite being non-cancerous, craniopharyngiomas can cause significant health problems due to their location and potential impact on nearby structures.
Craniopharyngiomas typically affect children and adolescents, but they can also occur in adults. The exact cause of these tumors is not well understood. They are thought to arise from remnants of the craniopharyngeal duct, which is a structure that connects the developing mouth and digestive system with the pituitary gland during fetal development.
The initial optimal treatment for craniopharyngiomas is maximal safe surgical removal. Fortunately for most patients, craniopharyngiomas can be removed through a keyhole route via the nose using an endoscopic endonasal approach or an eyebrow craniotomy.
Craniopharyngioma Neurosurgeons and Specialists
At Pacific Neuroscience Institute, located in Santa Monica, CA, we have one of the world’s largest experiences treating these tumors with endoscopic and keyhole approaches as well as treating residual and recurrent craniopharyngiomas.
By incorporating cutting edge technology and instrumentation with proven surgical experience, our surgical team led by neurosurgeons Drs. Daniel Kelly and Garni Barkhoudarian and ENT/otolaryngologist Dr. Chester Griffiths, strive to make craniopharyngioma surgery safer, less invasive and more effective.
Many if not most patients with a craniopharyngioma will need some form of pituitary hormone replacement and a significant minority may need radiosurgery or focused radiotherapy to prevent tumor regrowth. Our surgeons team works closely with our endocrinologists and radiation oncologists to provide optimal individualized care.
Given that some craniopharyngiomas cannot be removed completely by surgery or controlled with radiation therapy, tumor genomic profiling is being increasingly used to find alternative targeted therapies for these challenging tumors. In the case of papillary craniopharyngiomas, we also profile these tumors looking specifically for the BRAF mutation that may allow treatment with a targeted drug called a BRAF inhibitor.
Craniopharyngioma Overview
Craniopharyngiomas are benign brain tumors that arise near the Pituitary Gland and Pituitary Stalk and are typically both cystic and solid in structure.
They occur most commonly in childhood and adolescence and in later adult life, after age 50. They account for 10-15% of sellar and suprasellar tumors (tumors that occur in and above the pituitary gland) and 50-60% of sellar and suprasellar tumors in children.
They are usually not discovered until they impinge upon important structures around them, and are frequently quite large (over 3 cm) when detected.
Although they are benign (not malignant) tumors, these tumors tend to become adherent to structures around the pituitary gland and stalk, including the optic nerves, optic chiasm, intracranial arteries and the brain itself.
They are thought to arise from remnants of the craniopharyngeal duct or Rathke’s pouch which are developmental structures related to the primitive gut. They are thought to be closely related to Rathke’s Cleft Cysts (RCCs).
Symptoms of Craniopharyngioma
The clinical presentation of craniopharyngiomas can vary depending on their size, location, and the pressure they exert on surrounding structures. Common symptoms include headaches, visual disturbances, hormonal imbalances, growth abnormalities, weight changes, cognitive or behavioral changes, and increased intracranial pressure. The specific symptoms and their severity can vary widely among individuals.
Pituitary stalk compression
If the tumor compresses the Pituitary Stalk or Gland, the tumor can cause partial or complete Pituitary Hormone Deficiency which may lead to:
- Growth failure
- Delayed puberty
- Loss of normal menstrual function or sexual desire
- Increased sensitivity to cold
- Fatigue
- Constipation
- Dry skin
- Nausea
- Low blood pressure
- Depression
Pituitary stalk compression can also cause Diabetes Insipidus (DI), and increase Prolactin levels causing a milky discharge from the breast (galactohhrea).
Optic chiasm compression
If the tumor compresses the optic chiasm or nerves, then visual loss can result.
Hypothalamus
Involvement of the hypothalamus, an area at the base of the brain, may result in obesity, increased drowsiness and temperature regulation abnormalities.
Other symptoms
Other symptoms especially with larger tumors may include personality changes, headache, confusion, and vomiting. Large craniopharyngiomas which extend upward toward the fluid filled ventricles of the brain can cause hydrocephalus.
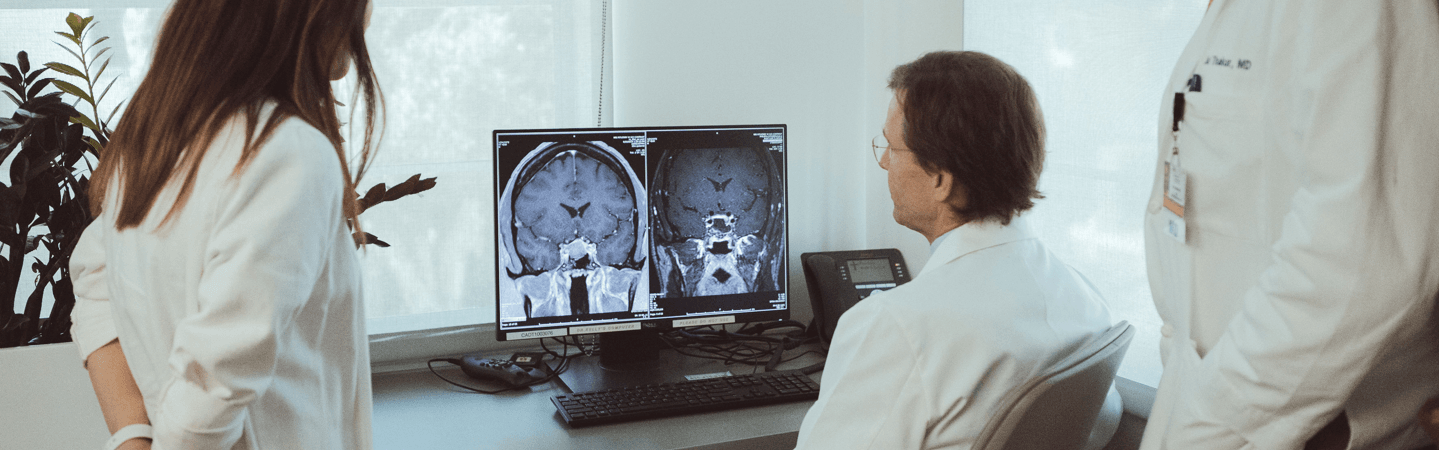
Diagnosing a Craniopharyngioma
Diagnosing craniopharyngiomas typically involves a combination of imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, to visualize the tumor and assess its size, location, and characteristics. Additional tests, including hormone assessments and visual field testing, may be performed to evaluate the tumor’s impact on hormone production and visual function.
While most craniopharyngiomas are easily diagnosed on MRI, sometimes they may be difficult to distinguish from other tumors or cysts that can arise in this region such as a cystic pituitary adenoma, a Rathke’s cleft cyst or an arachnoid cyst.
A complete pituitary hormonal evaluation should also be performed to assess for hormonal deficiencies which are quite common in patients with these tumors.
Craniopharyngioma Treatment
The treatment of craniopharyngioma involves a multidisciplinary approach, with input from neurosurgeons, radiation oncologists, endocrinologists, and other specialists. The treatment plan depends on various factors, including tumor size, location, the age and overall health of the patient, and the presence of symptoms or complications.
Overall Care
Because of their complex nature, craniopharyngiomas warrant a multidisciplinary approach that involves a highly experienced team that includes neurosurgeons, otolaryngolgists (ENT), endocrinologists, radiation oncologists and neuro-ophthalmoloigsts
Surgery
The best initial treatment for a craniopharyngioma is surgical removal. The goal of surgery is maximal safe tumor removal while improving vision and brain function and avoiding complications. If a patient has multiple pituitary hormonal deficiencies before surgery, it is reasonable to try for a more complete tumor removal. However, if pituitary function is largely normal, a more conservative surgical removal approach may be recommended in an effort to preserve gland function. The great majority craniopharyngiomas can be removed by either an endoscopic endonasal approach (through the nose) or a supra-orbital eyebrow craniotomy. Because of their tendency to be adherent to the optic chiasm, other nerves and important blood vessels, a total removal is possible in only 50 – 60% of patients.
Radiosurgery (SRS) or Stereotactic Radiotherapy (SRT)
With incomplete removal, stereotactic radiotherapy (SRT) or stereotactic radiosurgery (SRS), are typically used to prevent further tumor growth. Additionally, because of the tendency for craniopharyngiomas to recur, repeat MRI should be obtained at least every six months for the first 5 years after surgery or radiation and then at least annually thereafter.
Hormonal Replacement Therapy
Many patients with a craniopharyngioma will develop Pituitary Hormonal Deficits because of the tumor itself, surgery or as a result of radiotherapy. Such patients require hormone replacement therapy which may include thyroid, cortisol, testosterone (men), estrogen (women) and/or DDAVP for diabetes insipidus. Because hormonal deficiencies can develop years after radiotherapy, patients should have periodic hormonal evaluations throughout their lifetimes. Regular follow-up with an endocrinologist is recommended for all patients with a craniopharyngioma.
Doctors and Specialists Who Treat Craniopharyngioma
Patient Stories
Hear from our patients. Read their stories of courage and caring.
Craniopharyngioma: Brain Tumor Causing Visual Loss
When Odette, 47, from Denver, CO, found out she had a benign brain tumor called a craniopharyngioma, she didn’t hesitate to fly the over 800 miles to Southern California to meet with Daniel Kelly, MD, Neurosurgeon and Director of the Pacific Pituitary Disorders Center, to see what could be done.