Acromegaly 101: What To Know About the Disease, Diagnosis, and Acromegaly Treatment
by Daniel F. Kelly
This article on acromegaly is the second in a series on the diagnosis and treatment of pituitary adenomas and related hormonal disorders. Here we provide a brief overview of acromegaly, its manifestations and the optimal management including both surgical and medical advances.
What is Acromegaly?
Acromegaly is a rare, chronic condition that occurs when the pituitary gland produces too much growth hormone (GH) after the skeleton has finished growing normally. This causes bones, cartilage, organs, and other tissues to grow larger than normal, especially in the hands, feet, head, and face. Typical health issues that patients with acromegaly face are joint pain, cardiovascular problems, and diabetes. In children, the condition is called gigantism. In adults, it is called acromegaly. Treating acromegaly involves addressing the underlying hormone imbalance.
Causes of Acromegaly
While often described as a rare disorder, “relatively uncommon” may be a more apt descriptor of acromegaly. The disorder occurs fairly equally between men and women and can occur at any age but is more common in adulthood. If a child or adolescent develops a GH-secreting pituitary adenoma before their bones are fused, gigantism will develop. Gigantism is associated with excessive height, with many “pituitary giants” growing to over 7 or 8 feet in height.
In almost all cases, acromegaly is caused by a benign (non-cancerous) tumor of the pituitary gland (also known as the master gland) that secretes excess growth hormone (GH). The elevated blood GH levels cause the liver in turn to make excess insulin-like growth factor-1 (IGF-1), a hormone that has wide effects throughout the body. Surgery to remove a pituitary tumor is often needed to halt acromegaly.
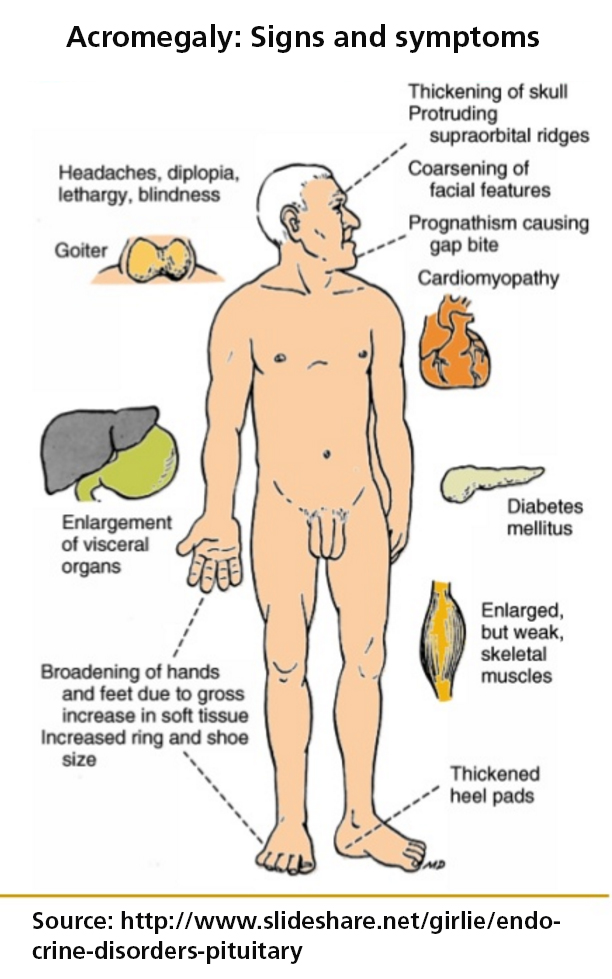
Symptoms of Acromegaly and Growth Hormone Complications
In patients with acromegaly, the elevated GH & IGF-1 levels can lead to numerous problems, many of which are manifested in one’s appearance and body habitus. These changes include enlargement of the hands and feet, enlargement and protrusion of the forehead (frontal bossing) and jaw (prognathism), temporomandibular (TMJ) syndrome, spreading of the teeth, increased facial hair in woman, as well as excessive sweating of the palms (hyperhidrosis).
Excess body fluid and tissue thickening can occur in the tongue and throat area– leading to snoring and obstructive sleep apnea–and in the hands leading to carpel tunnel syndrome. Even more serious for long term health is the increased risk of heart enlargement (cardiomegaly and cardiomyopathy), hypertension and diabetes as well as increased risk of colon polyps and colon cancer. Over time, untreated acromegaly results in an increased risk of death mostly related to associated cardiovascular disease and diabetes.
For patients with larger pituitary tumors (typically over 1.5 cm in diameter), there may be symptoms of visual loss from pressure on the optic nerves and optic chiasm, headaches and symptoms of pituitary gland failure (hypopituitarism) including low energy, low libido, loss of menstrual periods in women and weight gain.
The Two Major Challenges in Acromegaly Are:
1. Establishing a diagnosis
2. Effectively removing the adenoma and normalizing GH and IGF-1 levels
Diagnosing Acromegaly

The good news is that once pituitary-related acromegaly or gigantism is diagnosed, endonasal tumor removal of the pituitary tumor performed by experienced pituitary surgeons, has a very high success rate and safety record. Overall, 70-80% of patients with acromegaly achieve remission with surgery, and the resultant normalized GH and IGF-1 levels lead to resolution of many of the associated problems of the disease such as hypertension, diabetes, carpal tunnel syndrome, snoring and sleep apnea.
If surgery is not initially successful, use of medications is typically successful, and for the minority of patients who do not achieve remission with combination of surgery and medications, stereotactic radiosurgery (focused radiation) can lead to remission in the great majority of patients. These therapies need to be carefully considered, ideally in a multidisciplinary setting with a team of pituitary specialists, including neurosurgeons and endocrinologists.
We treat many patients with acromegaly who, in retrospect, had been having symptoms or signs of the disorder for years. Most commonly, these patients (or their significant others) notice their shoe size or ring size gradually increasing, increased snoring, or new skin tags on the back and torso. Some patients may also have been recently diagnosed with hypertension and/or diabetes. Finally, others might also complain of symptoms resulting from progressive tumor enlargement leading to pituitary gland failure and optic nerve compression — such as increasing fatigue and decreased libido, as well as headaches and visual loss.
Pituitary-related headaches are typically seen with large tumors and are generally localized to the forehead region or top of the head. Pituitary-related loss of vision typically manifests as decreased peripheral visual fields (aka bitemporal hemianopsia) and visual acuity.
Once the clinical suspicion of acromegaly has been raised, confirming the diagnosis is determined by blood testing of GH and IGF-1 levels, both of which will generally be elevated, although in some instances, GH levels drawn at random times of the day may be “normal”. As a result, in the setting of a normal GH level but elevated IGF-1 level, many endocrinologists will also perform an oral glucose tolerance test. During this test, an oral glucose drink is given, after which blood samples for GH are taken every 30 minutes for 2 hours. In normal individuals, GH levels are suppressed to very low levels, whereas in patients with acromegaly, the GH levels will not be suppressed after glucose intake.
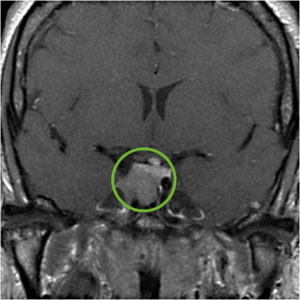
Following hormonal testing that confirms acromegaly, all the other pituitary hormones should be tested and an MRI of the pituitary with gadolinium contrast should be performed to confirm the presence of a pituitary adenoma. In the vast majority of individuals, an adenoma will be seen, typically a macroadenoma (larger than 1 cm in diameter).
For patients with visual complaints or a macroadenoma resulting in optic chiasm contact or compression on MRI, formal visual field testing by an ophthalmologist or neuro-ophthalmologist should also be performed.
First-line Treatment of Acromegaly – Endonasal Surgery
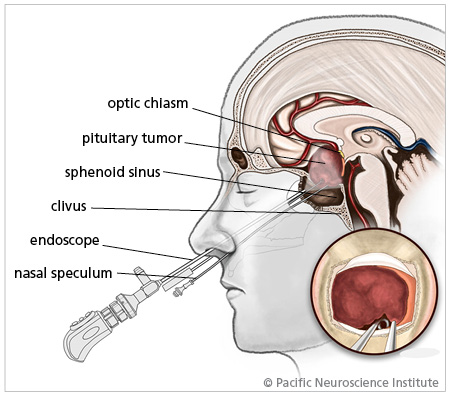
Fortunately, there are excellent treatments for acromegaly, starting with surgery, then medical therapies and lastly, focused radiation or radiosurgery. After diagnostic confirmation of acromegaly, endonasal transsphenoidal adenoma removal is considered first-line treatment. When performed by an experienced pituitary surgery team, long-term remission rates average 70- 80% and the risk of major surgical complications is very low, including a risk of new pituitary gland failure of less than 5%. The success rates are highest (typically greater than 85%) in patients with clearly defined non-invasive microadenomas (less than 1 cm in diameter) as seen on MRI. For patients with invasive adenomas, adenomas greater than 2 cm in diameter, or those with markedly elevated GH and IGF-1 levels, remission rates are substantially lower (typically ranging from 40-60%).
While we perform all of our pituitary operations using an endoscopic endonasal approach, studies to date have not been able to confirm that a purely endoscopic approach is better than a traditional microscopic approach (Starke et al 2013). However, several studies including our own (McLaughlin et al 2013) have shown the benefit and advantage of endoscopy for maximizing tumor removal, especially for larger tumors over 2 cm in diameter. Given that it is known that a greater percentage of GH-secreting tumor removal correlates with a higher likelihood of success with medical therapy in patients with acromegaly, we strongly recommend use of a fully endoscopic approach for all patients with acromegaly.
Most patients with successful surgery for acromegaly feel improvement within a day or two of surgery, primarily related to the rapid loss of excess tissue fluids, especially in their hands and feet. An early assessment of surgical success can be determined by measuring blood GH levels on day-1 after surgery, which should be less than 2 ng/ml within 24 hours given the very short half-life of GH. However IGF-1 levels fall more slowly and hit their nadir 6-8 weeks after surgery.
Long-term neurosurgical and endocrinological follow-up of acromegaly patients who achieve remission is strongly recommended given that late recurrences can occur, typically within 2-5 years after surgery but as late as 10-20 years after surgery. We typically follow our patients with blood levels of GH and IGF-1 and, for some patients, an oral glucose tolerance test every 6 months for at least 2-3 years post-surgery and then annually for at least 10 years.
Second-line Therapy of Acromegaly
What If Pituitary Surgery Fails and Acromegaly Persists?
For patients who do not achieve remission after transsphenoidal surgery, as evidenced by persistently elevated IGF-1 and GH levels, second-line therapy in most patients is therapy with injectable medications such as octreotide, lanreotide, pasireotide and/or pegvisomant. In a subset of patients with acromegaly, addition of an oral medication called cabergoline (Dostinex) may also be utilized. Cabergoline may be particularly helpful for patients who are proven to have GH and prolactin co-secreting tumors.
In patients whose MRI shows significant residual tumor or recurrence that is surgically accessible, and who have not had surgery by an experienced pituitary surgery team, repeat surgery may be a reasonable option before resorting to medical therapy.
In the small minority of patients who have not reached remission with surgery or medication therapies, stereotactic radiosurgery or stereotactic radiotherapy is the third option. For more detailed information on treatment options, recently released clinical practice guidelines are available: Acromegaly: An Endocrine Society Clinical Practice Guideline (Katznelson et al, J Clin Endocrinol Metab in 2014).
Radiosurgery for Acromegaly Treatment:
Radiosurgery is a non-invasive acromegaly treatment option. This precise technique targets and delivers high doses of radiation directly to the tumor, minimizing damage to surrounding healthy tissue. Radiosurgery, such as Gamma Knife or CyberKnife, is particularly useful for patients who cannot undergo traditional surgery or when residual tumor tissue remains after surgery. It offers a safer alternative with fewer complications, gradually reducing hormone levels and controlling tumor growth, making it an essential tool in the management of acromegaly.
Can you reverse the effects of acromegaly?
Reversing the effects of acromegaly involves early diagnosis and appropriate treatment. Acromegaly is caused by excessive growth hormone production, leading to enlarged tissues and organs. Effective treatment aims to control hormone levels and mitigate complications.
Treatment Options:
- Surgery: Often the first step to remove the tumor causing excessive hormone production.
- Medication: Includes drugs that reduce growth hormone levels or block its effects.
- Radiation Therapy: Used when surgery and medication are insufficient.
Therapy focuses on managing symptoms and preventing further complications such as diabetes, hypertension, and heart disease. Early intervention can significantly improve outcomes and reduce the severity of acromegaly’s effects.
How fast does acromegaly progress?
Acromegaly progresses slowly, often over several years, making early detection challenging. The gradual increase in growth hormone levels leads to noticeable changes in physical appearance and internal organ enlargement.
Progression and Symptoms:
- Physical Changes: Enlargement of hands, feet, and facial features.
- Internal Complications: Enlargement of organs such as the heart and liver, leading to severe health issues.
Does acromegaly affect personality?
Acromegaly can indirectly affect personality due to the physical and psychological changes associated with the condition. The excessive growth hormone can cause significant physical transformations and health issues, which can impact mental well-being and self-esteem.
Possible Effects on Personality:
- Physical Discomfort: Joint pain and headaches may lead to irritability.
- Emotional Stress: Changes in appearance can cause anxiety and depression and lead to social isolation.
- Health Complications: Chronic health issues, like diabetes and heart problems, can contribute to emotional strain.
Treating acromegaly involves managing both the physical and psychological aspects of the disease. Healthcare providers may use surgery, medication, and radiation therapy to control hormone levels and alleviate symptoms.
Does acromegaly affect the endocrine system?
Acromegaly significantly affects the endocrine system, disrupting the balance of hormones crucial for overall health. This disorder arises from excessive growth hormone production, usually due to a benign tumor on the pituitary gland.
Impact on the Endocrine System:
- Hormone Imbalance: Excessive growth hormone leads to abnormal growth of bones and tissues.
- Secondary Effects: Increased risk of diabetes, hypertension, and cardiovascular diseases.
In addition to the endocrine system, acromegaly can significantly affect metabolism due to the excessive production of growth hormone. This hormone imbalance disrupts normal metabolic processes, leading to various health issues that may need additional treatment strategies.
Metabolic Effects:
- Insulin Resistance: Increased growth hormone levels can cause insulin resistance, leading to higher blood sugar levels and an increased risk of diabetes.
- Weight Gain: Abnormal growth of tissues and changes in muscle mass can contribute to weight gain and altered body composition.
- Cardiovascular Issues: Metabolic changes may lead to hypertension and other cardiovascular problems.
Pacific Neuroscience Institute Experience in Acromegaly Treatment and Care

At our Pacific Pituitary Disorders Center, we have a long experience and academic track record in treating patients with pituitary adenomas and acromegaly in particular, including many patients with persistent or recurrent acromegaly. My personal series is over 2000 endonasal operations for all types of pituitary and related skull base and brain tumors, with approximately 80% of those cases being for pituitary adenomas.
We use an exclusively endoscopic endonasal approach due to the optimal visualization of the pituitary gland and related skull base anatomy afforded by the hi-definition endoscope. For every case we utilize high-definition cameras and monitors, 3D surgical navigation and Doppler probe for real-time carotid artery localization to maximize effectiveness and safety of the surgery. Our typical pituitary adenoma operation takes about 3-4 hours and most patients are discharged home within 24-48 hours of surgery.
Acromegaly Treatment Providers at Pacific Neuroscience Institute
Our Clinics
Given the complexities of diagnosis and treatment of acromegaly, it is critical that patients seek out a Pituitary Center of Excellence and use available patient and education resources. If you or a loved has symptoms of acromegaly see your physician or contact us at the Pacific Pituitary Disorders Center.
Pacific Neuroscience Institute – Santa Monica
2125 Arizona Ave., Santa Monica, CA 90404
310-582-7450
PNI-South Bay
5215 Torrance Blvd., #300, Torrance, CA 90503
424-212-5361
PNI-Burbank
501 S Buena Vista St., Burbank, CA 91505
818-748-4999
Useful Links
- Read what patients have to say about their experience in Part 2 of this two-part blog.
- Pituitary Network Association
- AcromegalyInfo.com
- Pituitary Society
- Hormones 411
Articles Related to Pituitary Adenomas
About the Author

Daniel F. Kelly
Daniel F. Kelly, MD, is the Director of the Pacific Brain Tumor and Pituitary Disorders Centers at Providence Saint John’s Health Center in Santa Monica, CA. Considered to be one of the top neurosurgeons in the U.S., Dr. Kelly is internationally recognized in the field of minimally invasive keyhole surgery for brain, pituitary and skull base tumors. He continues to focus his efforts on advancing innovative treatments for patients, providing fellowship training in minimally invasive neurosurgery, and patient education and support.
Last updated: August 22nd, 2024