What is an AVM?
by PNI Experts
What is an Arteriovenous Malformation (AVM)?
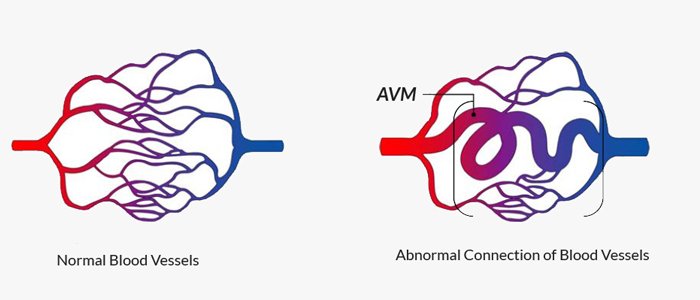
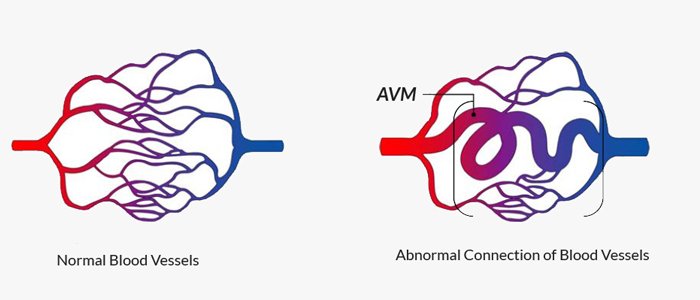
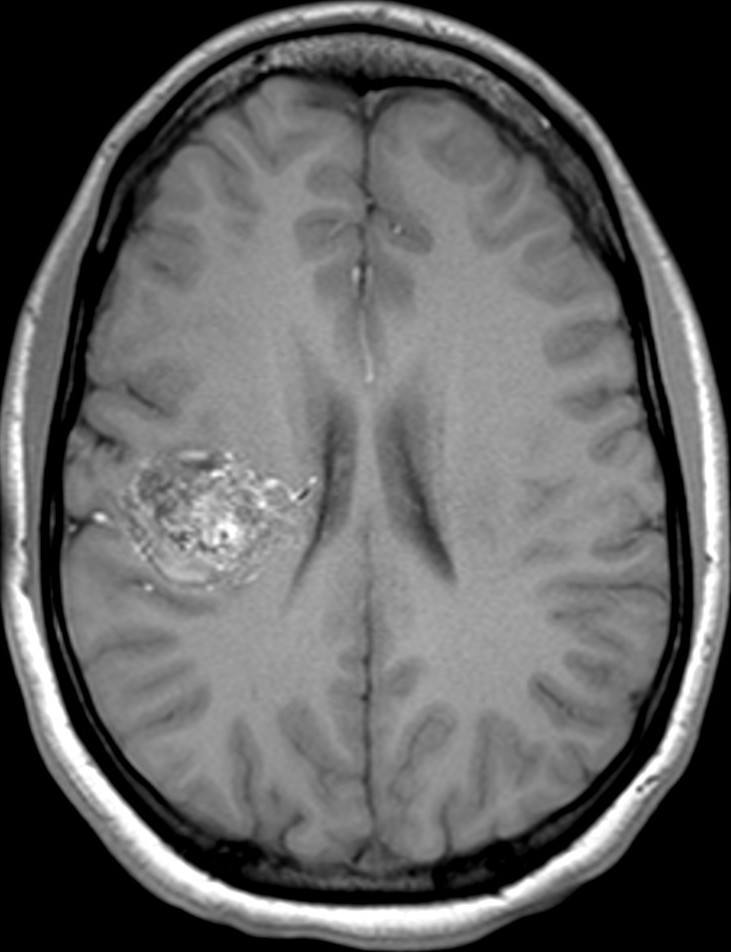
An arteriovenous malformation (AVM) is a tangle of abnormal blood vessels connecting arteries and veins in the brain. AVMs are a rare disease (approximately 1-5 out of 10,000 patients) of the blood vessels in the brain.
In healthy individuals, arteries that branch into smaller and smaller arteries carry high-pressure oxygenated blood to the brain. The exchange of oxygen occurs in tiny blood vessels called capillaries. Blood that is now low-pressure and has exchanged oxygen for carbon dioxide is then collected by small veins that then form larger veins and carry blood back to the heart and subsequently lungs.
In patients with brain AVMs, these connections are incorrect, and arteries in the brain connect directly to veins without the usual interspersed capillaries. This means that high-pressure blood ends up in veins, which are not built to withstand this pressure for a long time. In addition, the arteries usually are abnormally enlarged and tortuous, which is called the ’nidus’ of the AVM.
Are AVMs congenital or hereditary?
AVMs are thought to be congenital, and while not too much is known about this, most researchers believe they form in-utero or in the early postnatal period. However, only a small fraction of AVMs (about 5% ) are hereditary, for example in patients with HHT (hereditary hemorrhagic telangiectasia). Therefore, the vast majority of AVMs occur spontaneously and are not passed on from parents to their children.
Are there different types of AVM?
Brain AVMs are graded based on size, location, and venous drainage pattern to predict the treatment risk. This classification system is called Spetzler-Martin Grade and is used, in addition to other data, by the treating team of physicians to determine the optimal treatment strategy.
How are AVMs discovered?
Most AVMs at some point in the patient’s life become symptomatic. The most common symptoms are headaches, seizures, and bleeding in the brain due to AVM rupture. Less commonly, patients can also present with stroke-like symptoms that are possibly related to the AVM drawing away blood from adjacent normal brain. These symptoms often result in patients undergoing imaging of the brain with a CT or an MRI scan. Alternatively, we sometimes find AVMs ‘incidentally’, for example after a patient suffers from minor head trauma and a CT or MRI is obtained that then shows the AVM.
What causes AVM?
At this time we do not have a complete understanding of what causes AVMs. It is very likely that these lesions form in-utero or in the early postnatal period. For unknown reasons, AVMs occur more often in male patients. There are certain risk factors that predispose patients who carry AVMs to bleeding. These include a previous bleed, diagnosis at an older age, an certain anatomical features like an aneurysm in the nidus or narrowing of the draining vein that may increase the pressure in the nidus and vein proximal to the narrowing.
Symptoms of a brain AVM

The most common presenting symptoms of brain AVMs are related to bleeding in the brain due to AVM rupture, and symptoms can range from headaches only to neurologic disability (for example, one-sided weakness) and even coma or sudden death. Also common are seizures or chronic headaches. Less commonly, patients present with stroke-like symptoms but further tests show that the AVM has not bled; many experts believe that this situation is related to the AVM ’stealing’ blood from adjacent normal brain that is then without enough blood and oxygen to function properly. It is worth noting that 10-20% of AVMs are found ‘incidentally’, which means that a patient undergoes a CT or MRI for a reason unrelated to the AVM (for example minor head trauma), and these imaging tests then reveal the AVM.
Treating AVMs
There are three treatment modalities for brain AVMs.
- First, is microsurgical resection, where a neurosurgeon performs a craniotomy and resects the AVM nidus.
- Second, radiation therapy, where a radiation oncologist or neurosurgeon used a highly focused radiation beam to target the AVM nidus. The AVM nidus will then usually involute over the next several years.
- Third, embolization, where a neurointerventionalist injects a glue-like substance into the AVM nidus to decrease blood flow to the AVM.
For small AVMs that are surgically accessible, microsurgical resection is the treatment modality of choice. Similarly, for small AVMs that have not bled and that are in a deep location, radiation therapy is often chosen. For larger higher grade AVMs, a combination of these treatment strategies is often chosen. For example, a large AVM is often treated with embolization to allow for safe surgical resection or to reduce the size of the nidus and make the AVM treatable with radiation therapy.
Lastly, there is debate if AVMs that have not bled and are asymptomatic should be treated with these methods given the associated risks, especially with higher grade AVMs. Therefore, some patients are treated with medication to reduce the risk of bleeding, such as lowering the patient’s blood pressure, but the AVM itself is left alone. Especially in older patients with large AVMs that are in a deep location, this can be the best option.
Available diagnositics available at PNI
Pacific Neuroscience Institute has a multidisciplinary group of experts that are trained in the diagnosis and treatment of AVMs. Patients are often referred to PNI specifically for the treatment of brain AVMs, given that PNI has all available treatment modalities to individualize treatment and find the best treatment strategy for every patient.
Our AVM Experts
Contact Pacific Neuroscience Institute
Learn more about AVM treatment at our state-of-the-art facilities located at:
Providence Saint John’s Health Center
2125 Arizona Ave., Santa Monica, CA 90404
310-829-8319
Providence Little Company of Mary Medical Center Torrance
4201 Torrance Blvd., Suite 520, Torrance, CA 90503
424-212-5340
Useful Links
About the Author
PNI Experts
Last updated: March 3rd, 2023