

Streamlining Brain Tumor Surgery Care During the Pandemic
by Guest Author
BY PATRICIA AIDEM, Director, Public Relations, Providence Southern California
Pacific Neuroscience Institute at Providence Saint John’s strives to set new standard of safe, efficient, high quality minimally invasive brain tumor surgery during COVID-19.
SANTA MONICA (July 29, 2021) – In a first of its kind publication spawned by the forced opportunity of the Covid-19 pandemic, the Pacific Neuroscience Institute neurosurgical and otolaryngology surgical teams in collaboration with Providence Saint John’s Health Center, demonstrated a remarkable ability to dramatically reduce intensive care unit usage and days spent hospitalized for patients who underwent minimally invasive brain tumor surgery during the pandemic. The findings were published today in the journal PLOS ONE.
Winston Churchill is credited with saying “Never let a good crisis go to waste.” As U.S. health care eventually emerges from the pandemic, many aspects of surgical care, including how patients are prepared for surgery and where and how they recover will be forever altered. The pandemic’s strain on hospital ICUs and other facilities forced the PNI and Saint John’s teams to reconsider some basic assumptions about brain tumor care and acted as an accelerant to rapidly implement protocol enhancements that already had been in use on a more limited basis.
“Our findings suggest a streamlined care protocol can lead to marked reductions in ICU use and hospital length-of-stay without compromising patient safety or quality outcomes,” said neurosurgeon Daniel Kelly, MD, director of PNI and senior author of the study.
The pandemic-induced scarcity of ICU and monitored beds at our hospital further forced our clinicians and administrators to develop accelerated timelines and safety protocols from admission to discharge, so brain tumor patients with evolving neurological problems or endocrine/hormonal issues could be treated expeditiously.”
DR. DANIEL KELLY
“Brain tumor surgery by craniotomy or endonasal removal is resource intensive and historically has required multi-day hospital admissions, often including recovery in the ICU,” Dr. Kelly added. “For more than a decade, our PNI team at Saint John’s has been a leader and promotor of minimally invasive surgical approaches with “low impact” neuro-anesthesia, and strict complication avoidance protocols. The pandemic-induced scarcity of ICU and monitored beds at our hospital further forced our clinicians and administrators to develop accelerated timelines and safety protocols from admission to discharge, so brain tumor patients with evolving neurological problems or endocrine/hormonal issues could be treated expeditiously.”
The study involved 295 patients undergoing a total of 317 operations for brain, skull base or pituitary tumors, and compared two well-matched cohorts treated during non-overlapping 11-month periods (pre-pandemic versus pandemic.) The cohorts were divided further into patients who had craniotomies or endoscopic endonasal (via the nostrils) tumor removals.
“As our critical care team has treated several hundred COVID-19 patients and managed other critically ill patients during the pandemic, the ability to minimize ICU usage for non-covid patients and related resources was essential,” said Terese Hammond, MD, critical care specialist and Saint John’s ICU director. “This brain tumor protocol was extremely helpful and timely, showing how a concerted team effort can make substantive change for the safety of our patients and staff.”
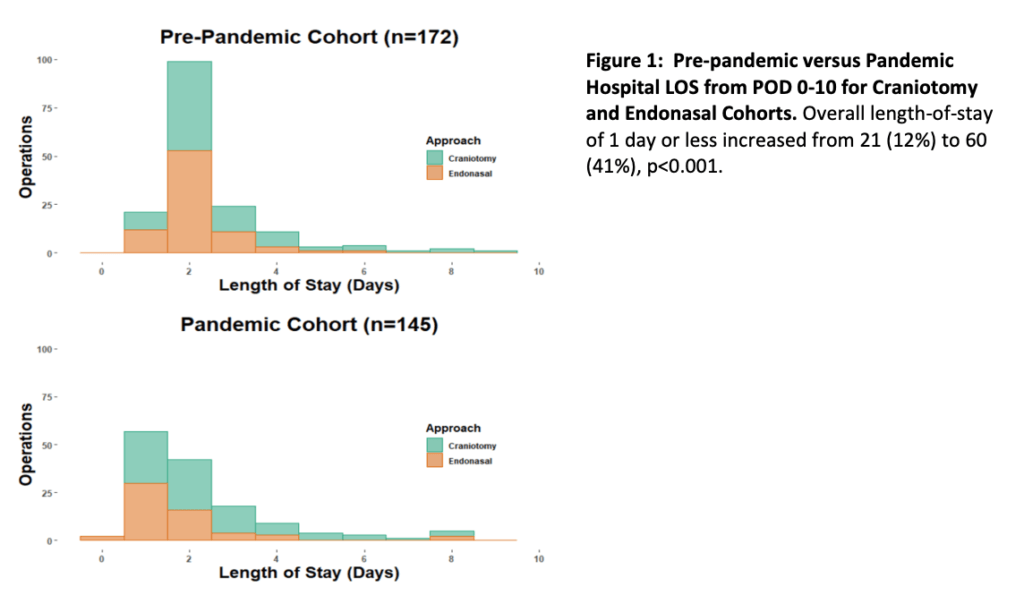
During the pandemic, the team implemented a streamlined care protocol of more rigorous patient education, more intensive recovery room assessment for safe admission to a non-ICU bed, earlier mobilization and post-discharge communication to facilitate less ICU use and earlier discharge. This protocol was associated with decreased ICU use from 54 percent to 29 percent of operations and hospital stays of one day or less increased from 12 percent to 41 percent. For the craniotomy cohort, median ICU stays decreased from one to 0 days and for the endonasal cohort, median hospital stays decreased from two days to one. There were no differences pre-pandemic versus pandemic in cohort tumor removal rates, complications, readmissions or reoperations.

“Not only was the care provided by our doctors and nurses exemplary, but the care protocol also has major implications for resource utilization and cost,” said Jared Amerson, Saint John’s chief operating officer. “We intend to continue this effort post-pandemic and will share our experience with other hospitals in the Providence system.”
Neurosurgeon Neil Martin, MD, PNI faculty member and regional director of neuroscience for Providence Southern California added, “We believe this streamlined care protocol, if integrated with rigorous minimally invasive surgery and complication avoidance paradigms, may be applicable to other brain tumor centers and more widely to other surgical specialties.”
About Dr. Daniel Kelly

Dr. Daniel Kelly, a board-certified neurosurgeon, is the Director and one of the founders of the Pacific Neuroscience Institute, Director of the Pacific Brain Tumor Center and Pacific Pituitary Disorders Center, and is Professor of Neurosurgery at Saint John’s Cancer Institute at Providence Saint John’s Health Center. Considered to be one of the top neurosurgeons in the US, he has one of the world’s largest series in endonasal surgery with over 2000 procedures performed including over 900 endoscopic endonasal surgeries, and almost 2000 craniotomies for brain and skull base tumors. In practice for over 25 years, he is a multiple recipient of the Patients’ Choice Award, and has been awarded the Southern California SuperDoctors distinction 15 years in a row.
Useful Links
Last updated: September 29th, 2021
