
Shining a Light on Facial Paralysis
by Guest Author
A new program at Pacific Neuroscience Institute helps an underserved population.
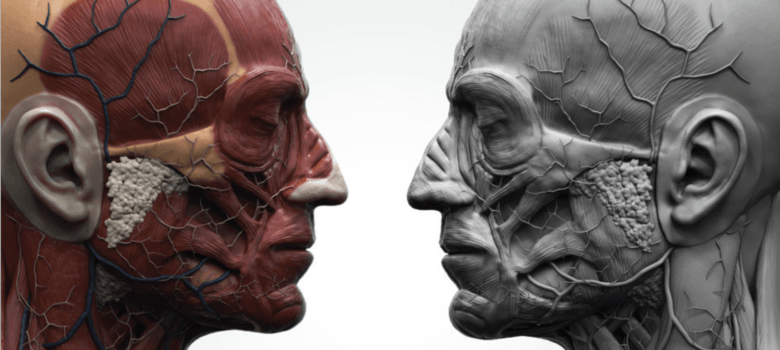
Facial paralysis can have a painful, debilitating effect—both physically and psychologically. Patients often have problems with eating, drinking, speaking and vision. Many patients feel disfigured, and the inability to smile or control their facial expressions may lead to isolation, depression and other emotional issues.
To provide these patients with the expert, compassionate care they need, Amit Kochhar, MD, has established the new Facial Nerve Disorders Program at Pacific Eye, Ear & Skull Base Center at Pacific Neuroscience Institute. As program director, Dr. Kochhar, who is double-board certified in otolaryngology–head and neck surgery as well as facial plastic and reconstructive surgery, wants to help what he feels is an “underserved patient population.”
Causes & Treatment of Facial Paralysis
Facial nerve damage may be caused by traumatic injury or result from surgery, particularly if it involves removing a tumor that is close to the facial nerve. Dr. Kochhar is one of a few select surgeons who performs complex, microvascular head and neck reconstruction to help these patients achieve better function and appearance—and results they are happy with.
“Data suggests that probably 30% to 40% of patients with facial paralysis who have been deemed ‘cured’ by their physicians still have some underlying disorder that goes unchecked,” says Dr. Kochhar, “often because their physicians don’t take their complaints seriously.”
According to Dr. Kochhar, physician education is key to ensuring these patients receive their desired level of care. “We’ve found that very few doctors understand how to manage facial paralysis—and on the West Coast, very few relative to the people who have it. That’s because most have not received sufficient training.”
“Dr. Kochhar offers a service that not many centers do, which is to take care of patients who have already had damage to the facial nerve,” says Garni Barkhoudarian, MD, chief of PNI’s radiosurgery program. “The necessity to have this type of service for our patients is truly critical.”
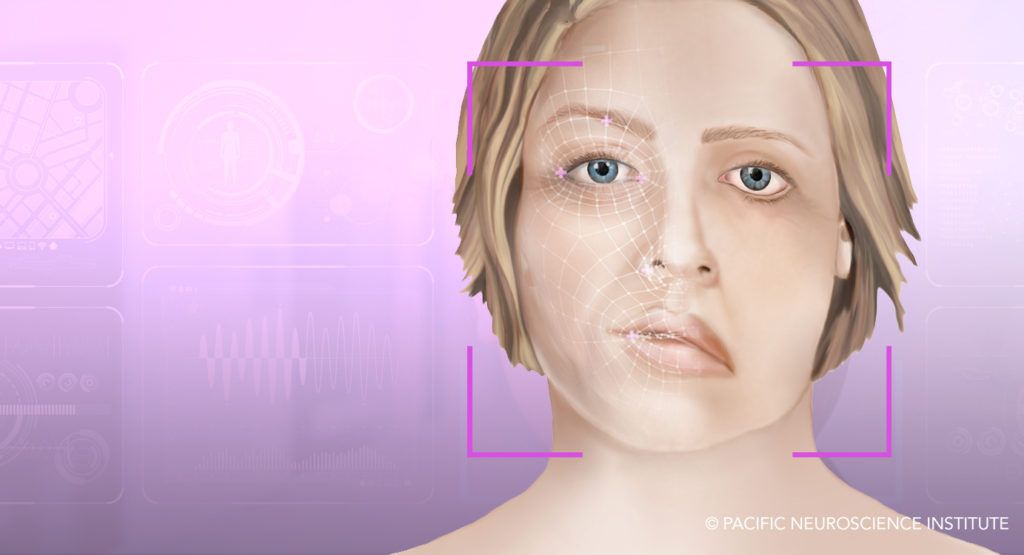
Facial Nerve Disorders Program Multidisciplinary Approach
Facial nerve disorders can also take other forms. For example, Bell’s palsy—a common form of facial paralysis from which patients typically recover—may result in secondary effects such as incomplete paralysis and synkinesis or involuntary muscle movements. Ramsay Hunt syndrome, or shingles of the face, can also result in facial paralysis that may take many months to recover. For patients with facial nerve disorders, Dr. Kochhar believes a multidisciplinary approach is key to their rehabilitation and the program’s success.
That is precisely why the Facial Nerve Disorders Program engages in a comprehensive approach that may include nonsurgical or surgical treatment, physical, occupational and speech-language therapy and consultations with neurosurgery and neuro-ophthalmology experts at Pacific Neuroscience Institute.
“We have incredible ancillary staff that can provide broad care for patients with facial paralysis,” Dr. Kochar says. “We are developing our own rehab program with facial, physical therapy and speech therapy. Having all of this under one roof will provide patients with the most optimal opportunity to be treated. I believe anyone can perform surgery to put nerves back together, but helping manage the patient through the recovery phase is the work of these incredible therapists.”
Shared decision-making between physician and patient is another important component when treating facial paralysis. Dr. Kochhar works to understand a patient’s No. 1 goal, followed by their secondary goals, to determine together the best course of treatment.
“A patient may come into my office and I can tell them about all the amazing options we can perform to help them smile again,” says Dr. Kochhar. “I can explain that I’m going to replace their nonfunctional facial nerve with the nerve they use to bite down or the nerve that moves their tongue. We can even transplant a muscle from their leg to help recreate the smile on their face. However, this doesn’t really matter if the patient is more interested in protecting their eyes so they don’t go blind. By employing a shared decision-making model, we can first address those primary goals and allow patients to appreciate the more complex options if they want to pursue them—not the other way around.”
Dr. Kochhar is grateful for the opportunity to create this program and collaborate with his world-class colleagues at PNI. “I don’t know any other group of doctors—and even the leadership at Saint John’s—that are so invested in doing this,” he says.
Another aim of the Facial Nerve Disorders Program is to educate physician partners in the community to be more comfortable identifying patients with facial paralysis and to refer them to PNI for patient-specific management, Dr. Kochar says. “I believe additional resources and research should be focused to identify specific goals for each patient individually to address their needs,” he adds. “Through philanthropic support of the Facial Nerve Disorders Program at PNI, we will not only be able to spread the word about our program’s efforts to help patients with facial paralysis, but we can also identify better ways to educate patients about their condition and how they can better move forward with their new faces.”
Facial Nerve Disorders Program: 310-829-8701
About Dr. Amit Kochhar

Amit Kochhar, MD, is Director of the Facial Nerve Disorders Program at Pacific Neuroscience Institute. He is double board-certified in Otolaryngology, Head and Neck Surgery and Facial Plastic and Reconstructive Surgery. He is one of a few select surgeons who perform complex (microvascular) head and neck reconstruction following cancer resections and facial trauma, as well as for the rehabilitation of facial paralysis, an area in which he has specific clinical expertise and research interest. In addition, he provides consultation for management of the aging face and nasal airway, and minimally invasive procedures for facial rejuvenation using laser, pulsed light, ultrasound, and radiofrequency energy.
By Laurel Digangi
Original article appears in Saint John’s Magazine, Winter 2020-21 issue
Last updated: January 23rd, 2021