What Can I Expect With Deep Brain Stimulation (DBS) Surgery? (Part 2/3)
by PNI Experts
In this three-part series, PNI experts at the Pacific Movement Disorders Center in Santa Monica and Torrance discuss deep brain stimulation (DBS) for Parkinson’s disease, essential tremor, and dystonia. Discover the most commonly asked questions about DBS and what to expect with DBS surgery.

- Preoperative evaluations
- What does DBS surgery involve?
- Components of the DBS system
- Surgical risks of DBS
- How is DBS surgery performed?
- Surgical targets for DBS
- Neurophysiology testing for DBS
- Mechanical guidance system
- Imaging
Whether it is enjoying a family meal, connecting with friends over the holidays, or pursuing your favorite hobby, Pacific Movement Disorders Center in Torrance and Santa Monica is here to help you improve in function and quality of life.
For patients with Parkinson’s disease, essential tremor, and dystonia, deep brain stimulation (DBS) surgery is highly successful and can improve tremor, rigidity and slowness, and symptom control.
DBS is a mainstream treatment methodology that is FDA-approved and covered by health insurance plans. Discover the steps before, during, and after the surgical procedure. As with any surgical procedure, there are some considerations.
What can I expect with deep brain stimulation (DBS) surgery?
Throughout the process, you will be followed by a neurologist and a neurosurgeon at Pacific Movement Disorders Center who have special training with DBS, as well as several other members of our team.
Preoperative Evaluations
Your neurologist/movement disorders specialist will evaluate you to see if you are a candidate for DBS. The evaluation may include some or all of the following:
- Medical history
- Neurological exam of your movements:

- MRI of the brain – to check for any issues with your brain that would prevent surgery. This scan is also used to plan the placement of your DBS electrode wires if you proceed to surgery.
- Lab tests – such as a blood test to make sure your blood clots properly.
- Neuropsychological tests – to test for underlying problems with thinking or talking that need to be considered during your surgery.
- Physical, occupational and/or speech therapy – to evaluate movement issues prior to surgery, including problems walking or taking care of yourself. Some individuals have swallowing problems before surgery that will be carefully evaluated by our speech therapists.
- Neurosurgical evaluation – you will meet with the neurosurgeon to review your exams and tests and discuss how DBS can help with your symptoms.
- Medical clearance – within 4 weeks of the procedure, you will need to have your primary care physician provide clearance from a medical standpoint. This may include EKG, Chest X-ray, or other tests.
Once the preoperative evaluation(s) are complete, your neurologist and neurosurgeon will discuss your case in detail.
What Does Deep Brain Stimulation Involve?
Deep brain stimulation therapy is completed in a series of steps. It involves both surgical and medical management by a team of neurosurgeons and neurologists. It can take up to 3 months to reach optimized therapy.
Stage 1: Fiducial (cranial) marker placement
This stage involves the placement of 4 cranial markers on specific points in the head. This will be done using a local anesthetic. The procedure is done in an outpatient procedure room, followed by a CT scan of the head. Patients are sent home after the procedure.
Stage 2: Lead implantation surgery
One to two weeks after stage 1, this stage involves implanting the leads in the brain. This is a precise brain surgery that is partially performed with the patient awake. The surgery takes part of a day and has multiple steps. At the conclusion of surgery, the lead(s) will be implanted in the brain and tested in the operating room to confirm its location. Most patients spend one or two nights in the hospital after this surgery, then return home for recovery.
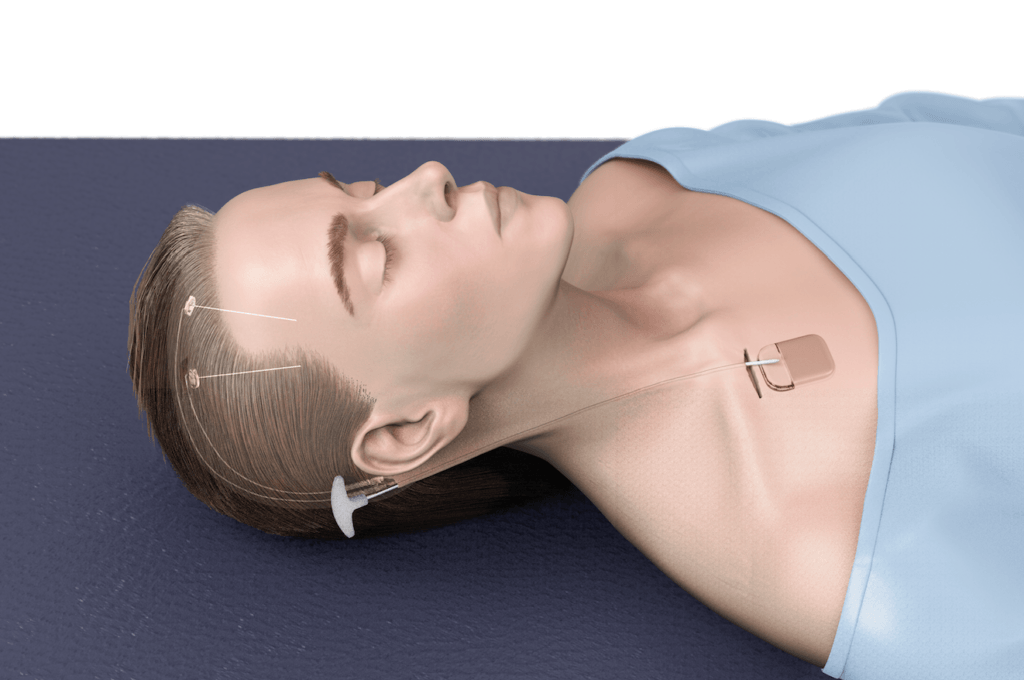
Stage 3: Generator implant surgery
One week after stage 2, this stage involves implanting the generator and extension wire to complete the system. The generator, also called the “battery,” is similar to a cardiac pacemaker. This procedure is performed under general anesthesia as outpatient surgery, and most patients go home the same day. A single generator is placed in the chest (outside the rib cage), which can connect to single or bilateral leads.
Stage 4: Programming the neurostimulator

The clinical benefit begins when the system is activated in the office. The first adjustment, or “programming,” is typically 1 to 3 weeks after the surgeries, when the patient has recovered and is back to their baseline. In the clinic, the stimulator settings are adjusted over multiple visits spanning up to 3 months. The neurology team also may modify medications while the system is increased and optimized over time. There will also be follow-up visits with neurosurgery to monitor the healing process. Keep in mind that deep brain stimulation is a process, and it may require weeks of follow-up and adjustments to the stimulator to achieve the maximum benefit. We encourage you to discuss your personal goals and expectations of the surgery with your neurologist or surgeon.
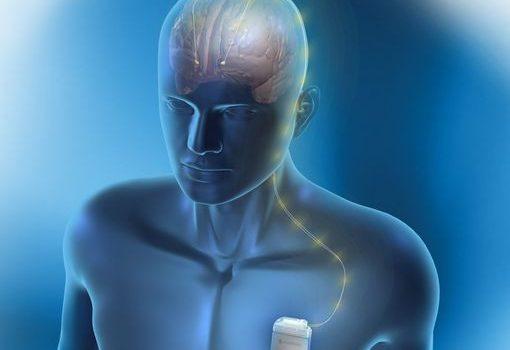
What are the components of the Deep Brain Stimulation system?
Leads
The lead is an insulated platinum-iridium wire, 1.8 mm in diameter, with several electrodes at the tip. The location in the brain for implantation depends on the medical condition. For Parkinson’s disease, the electrode is implanted in the subthalamic nucleus (STN) or the globus pallidus internal (GPi); for essential tremor, the tip is implanted in the ventral intermediate (VIM) thalamic nucleus; and for dystonia, the tip of the electrode is usually implanted in the GPi.
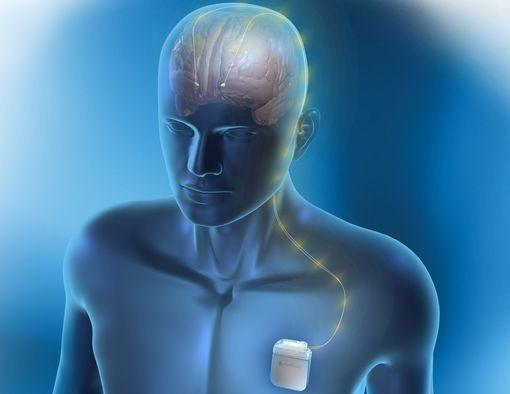
Extension Wire
The extension wire connects the lead and the generator. It runs under the skin from the scalp to the chest across the neck. It is rugged and can withstand movement.
Generator, “Battery”
The generator is a pacemaker-like device that powers the entire system. It contains a lithium-powered battery that has a computer chip programmed to send electrical pulses through the lead to control movement disorder symptoms. The battery generally has a two- to five-year life expectancy, depending on how high the parameters are programmed to control your symptoms. Rechargeable batteries are also available; these are rated to last 15 years.
Patient Programmer
You will receive a hand-held device that allows you to turn your stimulators on or off, check your battery life, and (in certain cases) make adjustments. Some essential tremor patients turn off their batteries at night while sleeping. For Parkinson’s and dystonia patients, batteries are left on all the time.
What are the surgical risks of Deep Brain Stimulation surgery?
DBS is a complex brain surgery that has risks. However, potentially serious major complications are uncommon. These risks include:
- Infection of the skin, hardware, and or brain.
- Bleeding in the brain (rare).
- Stroke (extremely rare).
- Worsening of neurological symptoms.
- Pain.
- Stimulation side effects include tingling, slurred speech, and balance difficulties. These can usually be reduced by modifying the DBS stimulation.
- Skin erosion over hardware.
- Mechanical damage to the DBS system or the stimulator.
How Is DBS Surgery Performed?
The goal of DBS surgery is to precisely implant the DBS electrode in a specific location deep in the brain. The target region is about 3 mm in diameter, so accuracy is critical. If the DBS electrode is placed off target then the therapeutic benefit will be less, and the stimulation side effects may be a problem.

There are many techniques and tools that are used to improve accuracy: 1) choose the target, 2) guide the electrode through the brain to the target, and 3) confirm the electrode is in the correct location. The techniques used in DBS surgery are rapidly evolving. Each patient has different disease status and preferences. These factors are considered when the patient and surgeon decide together how to perform the surgery. In general, the following are different techniques and options in DBS surgery.
Surgical Targets
There are three common target locations in DBS surgery: subthalamic nucleus (STN), ventrointermedius nucleus of the thalamus (VIM), and posteroventral globus pallidus internus (GPi). The target of your surgery depends on your disease.
- Essential Tremor: The target is almost always in the VIM. This is clearly the best location for tremor control, even in Parkinson’s disease, and sometimes in dystonia. The VIM target is within 2 mm of the sensory nucleus of the thalamus. Stimulation at high intensity causes paresthesia – tingling. It can also cause slurred speech, particularly common in bilateral surgery.
- Dystonia: The GPi is the most common target in dystonia. Typically, DBS electrodes are inserted bilaterally at the same time. This target is effective for nearly all types of dystonia. On occasion, the STN or VIM are used.
- Parkinson’s Disease: The STN is the most common target, but often the GPi is used. It depends on the symptoms. If tremor is the major symptom the STN is a better target. If dyskinesia is the major symptom, then the GPi is a better target. STN DBS tends to result in greater medication reduction than GPi. Otherwise, either location has a similar benefit. The target in your case is chosen by both the movement disorder neurologist and neurosurgeon, considering your preference as well.
Neurophysiological Testing
The deep structures in the brain including the target region have specific neurophysiological characteristics that can be monitored and tested to confirm the DBS electrode is in the correct location. The following is a list of techniques commonly used. Many of these techniques are combined in one surgery.
- Microelectrode mapping: A thin wire called a microelectrode is passed through brain structures including the target. This microelectrode is like a microphone, and it listens to individual neurons. The pattern of neuron activity is different between brain structures. Historically this has been the most widely used technique.
- Beta-Band: The DBS electrode can be used to listen for certain patterns and frequencies of activity. The beta-band signal is commonly found at the target region in many patients with PD. It is thought to be a neurophysiological signal of disease. DBS stimulation and medications appear to reduce this signal. The beta-band can be monitored in surgery, and new generation DBS generators are able to monitor this after surgery.
- Macrostimulation: Therapeutic stimulation through the DBS electrode can be performed in the operating room. The clinical effect on your disease condition such as tremor, slowness, and stiffness can be determined. This helps to confirm that the DBS electrode is in the correct location. Just as important is the measurement of DBS stimulation side effects, and at what stimulation intensity they occur. These side effects include paresthesia – a tingling sensation, dysarthria – slurred speech, and contractures – muscular pulling of the face or hand. If these side effects occur at too low of a stimulation intensity the DBS electrode may be moved. This is the purpose of the awake stage of brain surgery.
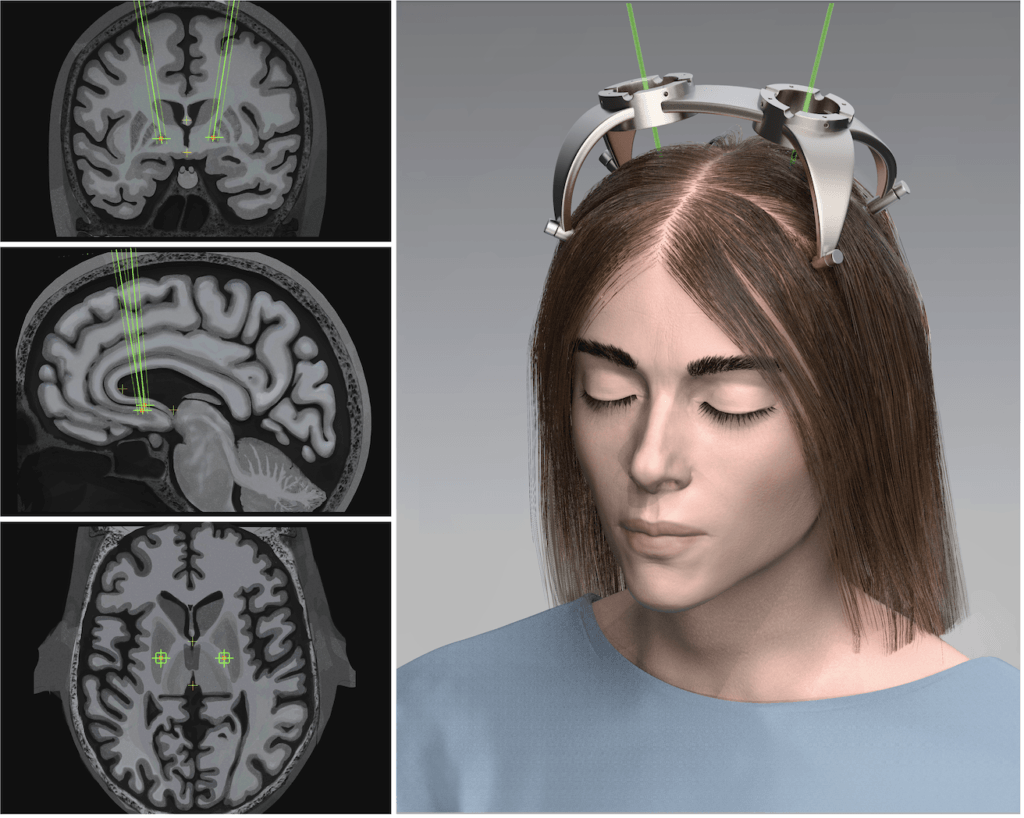
Mechanical Guidance System
In every case, the surgeon uses a mechanical guidance device to place the DBS electrode. All of these devices attach to the skull and provide mechanical stability and accuracy. Historically DBS has been performed with a “frame.” This is a halo device that is attached to the skull, and a system then fastens to the halo and guides the electrode. The frame is connected to the operating table to prevent the patient’s head from moving.

Center.
At PNI, we instead use customized patient-specific plastic frames to guide the electrode. These systems are termed “frameless” because they do not use a halo, even though they still use a guidance system. This allows the patient’s head to move during the procedure, as the guidance system will move with the head. This approach, which we take at PNI, allows for a shorter procedure as both leads can be implanted simultaneously, and has been shown to be as accurate as frame-based procedures.
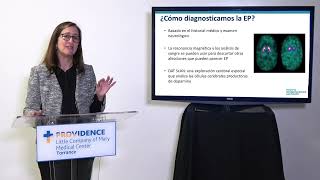
Imaging
Imaging is playing a more crucial role in DBS surgery. New high-quality MRI scans are used for preoperative targeting.
Useful Links
- What Is Deep Brain Stimulation? (Part 1/3)
- 25 Questions About Deep Brain Stimulation (Part 3/3)
- Parkinson’s Disease
- Dystonia
- Essential Tremor
About Pacific Movement Disorders Center
Pacific Movement Disorders Center offers surgical and non-surgical options for movement disorders. Properly managing movement disorders must include both education and support. With informational programs, support groups, psychological care, and caregiver guidance, we’re with you at every step. Our partnership with American Parkinson’s Disease Association (APDA) also provides structured support groups for newly diagnosed PD patients and their families.
Pacific Movement Disorders Locations

The Pacific Movement Disorders Center’s state-of-the-art facilities are located at:
Providence Saint John’s Health Center
2125 Arizona Ave, Santa Monica, CA 90404
310-829-8265
Providence Little Company of Mary Medical Center Torrance
5215 Torrance Blvd, Suite 300, Torrance, CA 90503
424-212-5361
Meet the Team
About the Author
PNI Experts
Last updated: February 8th, 2023