
Deep Brain Stimulation (DBS)
The goal of deep brain stimulation surgery is to modulate the activity of a specific brain region.
In Parkinson’s disease, essential tremor, and dystonia, normal function can be restored to the circuitry of the brain, resulting in significant improvement in function and quality of life.
What is deep brain stimulation (DBS)?
In DBS, thin electrodes are placed in the disruptive areas of the brain and small electrical pulses normalize or eliminate the irregular signals. DBS is the non-permanent suppression of overactivity in the autopilot structure of the brain called the basal ganglia.
Like a pacemaker for the brain, the battery (pulse generator) is implanted under the skin of the chest, and leads (wires) are tunneled under the skin via the deep part of the brain through a quarter-sized opening in the skull. The system is fully implanted under the skin, so there are no external wires or devices. The stimulator is fully programmable and therefore adjustable over time, as the disease changes. Patients can use a simple hand-held device to turn the DBS on or off, and adjust various other parameters if needed.
The procedure is done in three steps:
- The placement of leads: During this procedure, patients are mildly sedated and given local anesthetic to numb the skin. Because the brain tissue itself has no pain receptors, the leads can be placed with patients awake. This allows our team to determine the benefits of the stimulation. Patients typically stay one night in the hospital and are discharged the following day.
- This procedure can be done with a frame (frame-based) or without a frame (frameless). Although we can perform a frame-based approach, the use of the frameless option provides a significantly more comfortable experience for the patient. Instead of having to wear a rigid frame that gets screwed into the operating table, immobilizing the head and neck, the frameless system is attached to the skull via previously placed fiducial markers, allowing the head and neck to remain mobile. The system employs a custom-made mini frame fitted to the patient’s head which reduces the time required for the surgery therefore optimizing recovery, without compromising precision.
- The placement of the pulse generator battery: This is done under general anesthesia, and typically 1-2 weeks after lead implantation. The pulse generator needs to be replaced about every 3-4 years. A rechargeable option exists that lasts 9 years but requires regular charging. At the post-operative visit, the battery is turned on and DBS programming begins. While it may take a few weeks for maximal benefit, patients soon experience relaxation of symptoms. The DBS program is customized for each patient based on maximizing symptom reduction.
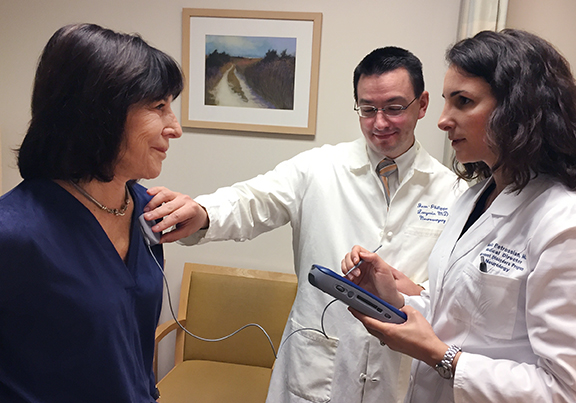
- The programming of the neurostimulator: About 3 weeks after the battery implantation, patients come to the office for activation of the DBS system. The settings are adjusted gradually and several configurations are tested to find the optimal settings at the first visit. It may require weeks of adjustments to medications and DBS settings to achieve the maximum benefit of both.
What DBS candidates should consider:
How Can DBS Help Me?
For Parkinson’s Disease (PD)
In patients with PD who have motor complications, dyskinesias, or tremor not improved with medication, DBS improves ON time, reduces dyskinesias and reduces tremor.
For Essential Tremor (ET)
In patients with ET who have tremor interfering with activities of daily living such as pouring liquids, drinking from a cup, or writing, DBS dramatically reduces tremor and improves quality of life.
For Dystonia
DBS reduces dystonia, improves quality of life and improves ability to perform activities of daily living in patients with medication-refractory dystonia, including both generalized dystonia and cervical dystonia.
Benefits of DBS
For patients with Parkinson’s disease, one of the main advantages of this kind of therapy is that medication fluctuates over time while DBS remains constant throughout the day. DBS is always on and complements an optimized medication regimen. Because DBS remains active between medication doses, it helps patients sustain longer periods of symptom-free activity even after the medication’s effect has worn off. On average, patients gain four to five hours of productive time in a typical day with DBS. It improves the main symptoms of Parkinson’s disease including tremor, rigidity and slowness and has been shown to improve quality of life. DBS is a mainstream treatment methodology that is FDA-approved and covered by health insurance plans.
DBS can have a transformative effect on quality of life for patients with essential tremor because of the high rate of symptom control. The vast majority of patients experience a significant improvement in tremor allowing them to perform their work or their hobbies. Our patients tell us they are finally able to enjoy meals with family and friends again as tremor symptoms remains under control.
The use of DBS for patients with dystonia improves objective scores of dystonia movement and disability, but more importantly, it greatly improves quality of life including physical function, pain, general health and depression scores.
Potential Risks of DBS
- DBS surgery is highly successful and as with any surgical procedure, there are some considerations. Post-operative headache and pain is possible which typically resolves gradually within a few weeks of the procedure. Neck pain may manifest in the short term. Infection of the leads, extension or battery is very low risk. Hemorrhage is extremely low risk but when it occurs may lead to stroke-like symptoms which alleviate and do not result in permanent complications. Lead fracture or migration, also very low risk, may require repeat surgery.
- Problems with speech, language and mood, muscle tightness, slurred speech and vision symptoms can be related to the stimulation and thus can usually be reduced or eliminated by adjusting the stimulation.
