Hemifacial Spasm
Hemifacial spasm is a condition with twitches or spasms of one side of the face, often starting with one eye and spreading into the cheek or lips.
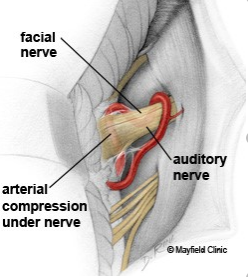
Patients often describe the movements as tics but to be exact, the movements are not true tics, which are semi-involuntary movements in response to an irresistible urge to move. The movements in hemifacial spasm are truly involuntary, though they can be triggered by stress or eyelid closure. Hemifacial spasm typically is caused by an artery pressing on and irritating the 7th cranial nerve, known as the facial nerve. It can also occur after Bell’s palsy or other 7th nerve conditions.
Diagnosis
Hemifacial spasm is a clinical diagnosis based on an examination of the movements of the face. MRI of the brain is obtained with thin cuts through the brainstem where the 7th cranial nerve runs, as well as an MRA (non-invasive angiogram) of the arteries of the brain.
Treatment
Botulinum toxin works to partially block the communication between the nerve and the muscle, thereby relaxing overly active muscles. We utilize EMG (electromyography) guidance to target the most active fibers within the muscles of the lower face. The procedure takes about 20-30 minutes and may be associated with pain and bruising but this is typically temporary. Botox takes 3-10 days to kick in and lasts 3-4 months, meaning that most patients return for repeat injection 3-4 times per year.
Botox is covered by insurance for treatment of hemifacial spasm. Treatment of the eye spasm often is sufficient to treat the lower face spasms as well. The main side effect of Botox is weakness of eye closure causing dry eye or tearing; if lower facial injections are required side effects can include asymmetric appearance or drooping of the face. Rare side effects include eyelid droop, double vision, and trouble swallowing. Botox is temporary so side effects would resolve after 2-3 months.
Oral medications used for hemifacial spasm include clonazepam (benzodiazepines) and Artane (trihexyphenidyl), but these can be sedating, so injections are preferred.
For patients who have not responded favorably to injections with botulinum toxin, or in whom side effects limit their use, consideration of surgical treatment, namely microvascular decompression is an option.
Microvascular Decompression
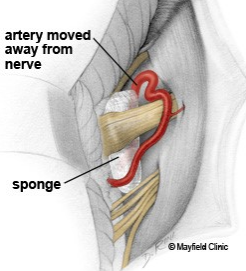
The procedure to move the artery and decompress the nerve – a microvascular decompression – is performed via a keyhole endoscope-assisted craniotomy using minimally invasive techniques, so there is only a 1.5-inch scar behind the ear. The artery is carefully moved away from the facial nerve and a small amount of Teflon is placed in between to protect the nerve from further irritation.
Microvascular decompression has a cure rate between 85-95% and a complication rate of less than 3%, including transient or permanent hearing loss, CSF leak, or transient or permanent facial weakness. Patients typically spend a night or two in the hospital, and Post-operative recovery is typically 2-3 weeks.