
7 Questions About Bell’s Palsy
by Garni Barkhoudarian
Bell’s palsy is the most common cause of facial palsy (paralysis of the face). Thankfully, the majority of patients will recover to normal or near normal facial nerve function.
1. How/when is Bell’s palsy diagnosed?
This condition occurs suddenly, most often without propagation, though it has been associated with immunosuppression, stress and viral illnesses (e.g. influenza).
2. What are the risk factors for contracting Bell’s palsy?
This condition can affect both genders equally, though pregnancy does increase the risk 3-fold. Patients with diabetes, hypothyroidism and the elderly are at higher risk as well. Often, a viral infection precedes Bell’s palsy by 1-2 weeks. It is thought that such an illness can trigger Herpes virus (which typically sits dormant in the facial nerve cell body) to activate and cause painless facial weakness.
3. What types of symptoms are associated with Bell’s palsy?
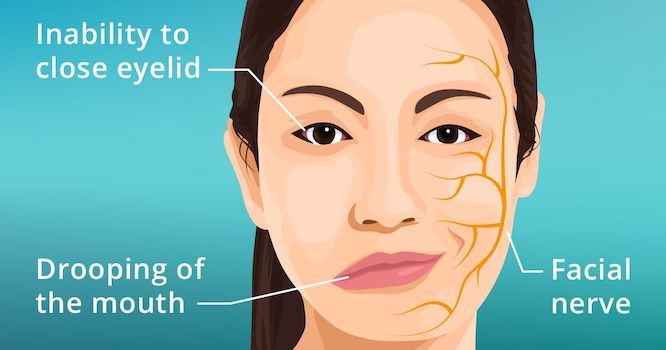
Bell’s palsy patients will experience their entire face weaken or become completely paralyzed.
This includes inability to blink or close the eye, smile symmetrically, or chew food. This is in contrast to stroke victims, where only the lower part of the face (mouth and cheek) will be weak, with preservation of eye function.
In addition, patients may complain of :
- Ringing in the ears (tinnitus)
- Hearing sounds louder on the affected side (hyperacusis)
- Decreased sense of taste on the affected side of the tongue
- Decreased salivation / tearing on the same side of the face
It is very important to note that Bell’s palsy is a diagnosis of exclusion. This means that other causes of facial weakness such as stroke, brain tumor, Guillan-Barre syndrome, ALS, trauma, post-surgical, infection, etc., should be ruled out.
Hence, a thorough evaluation of the entire body, as well as laboratory work-up and neuroimaging (MRI), is necessary before concluding one has Bell’s palsy.
4. How does it progress?
The typical course of Bell’s palsy is a sudden or rapid onset of facial weakness or paralysis over 1-2 days. This will typically last for a few weeks, with patients starting to recover facial function typically around 3 weeks, though recovery may take up to 9 months.
5. What treatments are available?
The first-line treatment option for Bell’s palsy is corticosteroids (e.g. prednisone). This has been shown to help the rate of recovery. Often, physicians will also prescribe antiviral medications simultaneously, given the proposed mechanism of Herpes virus reactivation causing the facial weakness.
In severe, refractory cases, surgical decompression of the facial nerve may be indicated, though this is significantly riskier and it is unclear whether there is any clinical benefit. Acupuncture and electrical stimulation of the facial muscles have also been used with some success.
6. What are the side effects of Bell’s palsy and/or its treatment?
The majority of patients receiving steroids will have short-term side effects (most of which resolve once the medication is halted, including insomnia, weight gain, gastritis and mood changes.
In diabetic patients, steroids can worsen blood sugar control and may require higher doses of insulin and other medications. Long-term (more than a few months), steroids can result in immunosuppression, easy bruising, wound breakdown, bony fractures or necrosis, cognitive changes, diabetes and high blood pressure.
Though the majority of patients will recover well, up to 30% of patients may develop permanent partial facial weakness, dry eyes and diminished taste.
It is imperative during the duration of severe facial weakness that the affected eye is protected (as the blink reflex is absent/unable to protect the eye). Corneal abrasions can occur if the eye is not kept safe, and blindness may result. Hence, the eye should be covered at night with an eyepatch or a piece of tape. During the day, the eye can be left uncovered, but artificial tears should be used copiously to prevent scleritis.
7. Is there is a cure or remission period?
Most patients will be cured once the facial palsy resolves. However, in up to 12% of patients, recurrence may be noted, with multiple recurrences affecting about 3% of patients.
For more information about facial syndromes, contact Dr. Amit Kochhar, Director of the Facial Nerve Disorders Program at the Pacific Eye,Ear & Skull Base Center. 310-829-8701 or schedule an appointment online.
Image credit: allaboutvision.com
About the Author

Garni Barkhoudarian
Dr. Garni Barkhoudarian is an expert neurosurgeon and director of the Facial Pain and Adult Hydrocephalus Centers, and Co-director of the Pituitary Disorders Center at Pacific Neuroscience Institute. His philosophy for virtually all intracranial procedures is to apply the keyhole concept of minimizing disturbance to the brain and its supporting structures.
Last updated: June 3rd, 2022