
The Power of Immunotherapy
by Santosh Kesari
Our immune systems hold the power—the power, that is, to treat cancer. Composed of various types of cells, tissues, and organs, the immune system serves as more than the body’s main defense against foreign invaders such as bacteria and viruses. It also recognizes cancer cells as foreign invaders and eliminates them too.
And while the immune system is often successful at destroying cancer cells, sometimes the defense is not able to find the cancer cells or keep up especially as we age. So, the cancer cells continue to multiply, eventually forming a tumor.
Boosting the Immune System
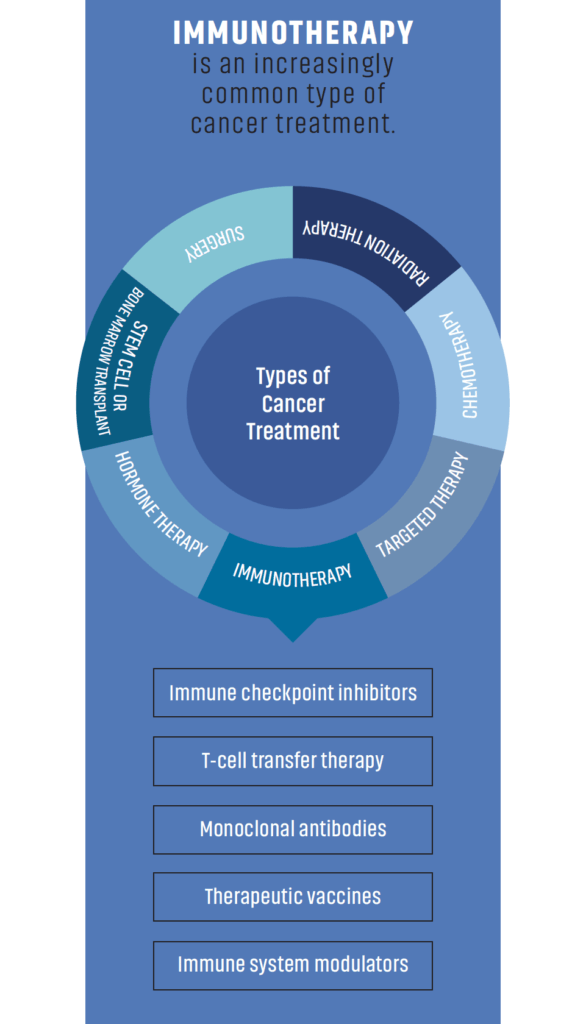
The good news is researchers are harnessing the immune system’s natural ability to fight cancer by developing drugs that boost the immune system. These drugs are known as immunotherapies and there are three main types: nonspecific immune stimulation, immune checkpoint inhibitors, and adoptive T cell transfer therapy.
- Nonspecific immune stimulation involves drugs that activate the immune system in a general way to kill cancer. For example, Bacillus Calmette-Guérin can be used to eliminate bladder cancer cells that may remain after surgery to remove the bladder cancer. In addition, three substances that are naturally produced by the immune system—interleukin 2, and interferon-alpha and colony stimulating factors —can be used to activate specific cells in the immune system to treat types of cancer.
- Immune checkpoint inhibitors are an increasingly common treatment in cancer. They don’t target the tumor itself but instead work by removing the “brakes” of the immune system. As a result, an immune cell known as a T cell becomes activated and eliminates cancer cells. Several types of immune checkpoint inhibitors have been approved for use across many cancer types. Pembrolizumab, nivolimab, and ipilimumab are common types of immune checkpoint inhibitors.
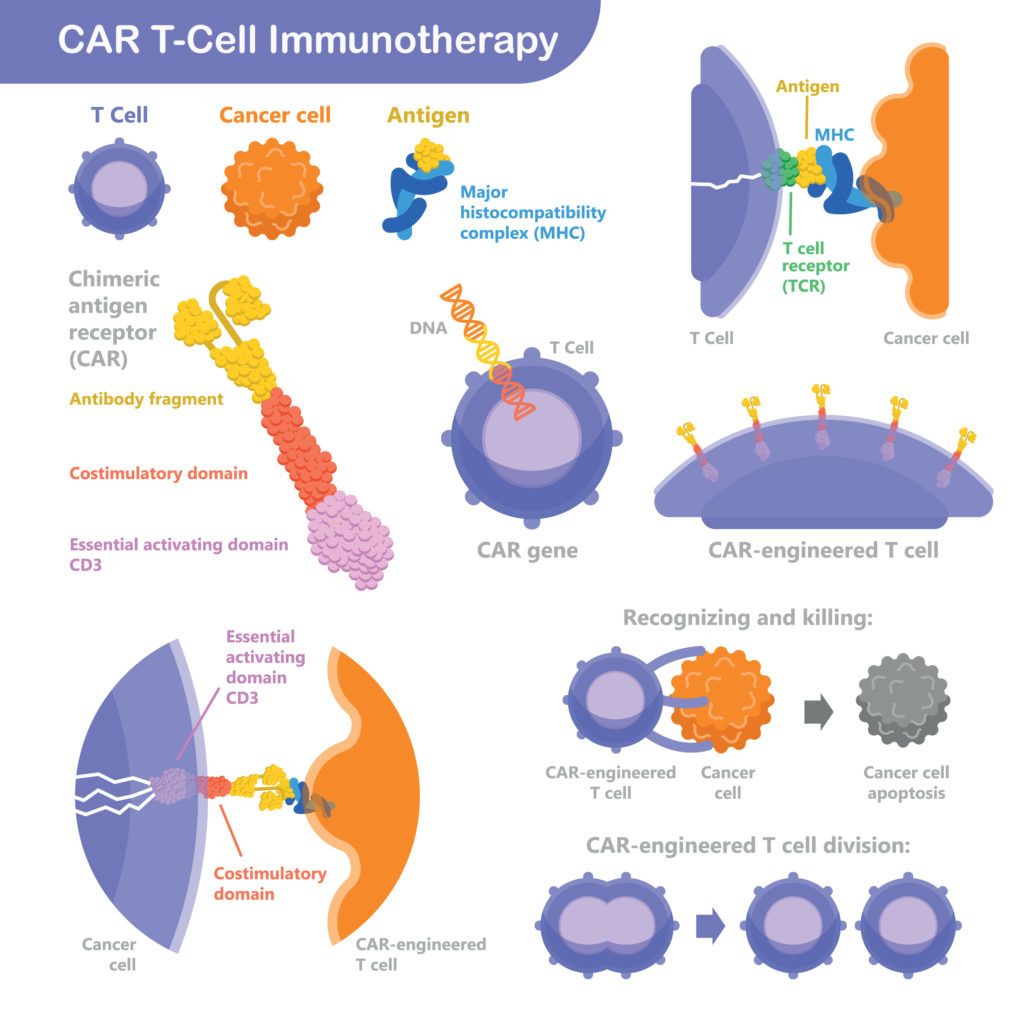
- Adoptive T cell transfer therapy is a newer form of immunotherapy and is often referred to as CAR T-cell therapy. This approach, like immune checkpoint inhibitors, also involves using the T cells to attack the tumor. But a key difference is a portion of these T cells are first removed from the patient’s body and re-engineered in a lab to target the tumor. The re-engineered T cells are then infused back into the body, where they home in on the cancer cells and destroy them. Currently three CAR T-cell therapies are approved for certain types of blood cancers and many more are in clinical development for other types of cancer.
Immunotherapy is considered such a significant advance for cancer treatment that the 2018 Nobel Prize in Physiology or Medicine was awarded to two cancer immunotherapy researchers, James P. Allison, PhD, of The University of Texas MD Anderson Cancer Center, and Dr. Tasuku Honjo of Kyoto University in Japan. Together, their work led to the development of several immune checkpoint inhibitors that are used in cancer treatment today.
Immunotherapy and Brain Cancer
While immunotherapy has become a common treatment in cancer types such as lung, kidney, and melanoma, it’s had limited success for brain cancers. In general, brain cancers are difficult to treat with drugs because the brain is shielded by a membrane called the blood-brain barrier.
As the name implies, the blood-brain barrier selectively blocks the types of substances that can enter the brain through the bloodstream. This barrier helps keep harmful substances, like bacteria, out of the brain but also means it can keep helpful ones, like cancer drugs, from reaching a brain tumor.
Research is Underway
At the Pacific Neuroscience Institute, our neuro-research and clinical trials teams, and research doctors at the Saint John’s Cancer Institute at Providence Saint John’s Health Center, Santa Monica, help conduct research studies to develop immunotherapy treatments for patients with brain cancer.
For example, we have a brain cancer study that launched in 2018 at Pacific Neuroscience Institute, Saint John’s Cancer Institute, and Providence Saint John’s Health Center. The study is known as Precision Immunotherapy in the Neoadjuvant Setting (PIN).
The study evaluates immunotherapy options in volunteer patients with newly diagnosed glioblastoma, a highly aggressive type of brain cancer. The idea is that treating patients with immunotherapy before they receive standard radiation and chemotherapy ensures that their immune systems are more robust and thus better equipped to kill a tumor.
In addition, there is a study that assesses immune checkpoint inhibitors in volunteer patients with newly diagnosed high grade glioma before they receive radiotherapy. Brain tumor samples are collected throughout the study to help identify unique characteristics in patients who respond to treatment.
The results, published in the most recent edition of Journal for ImmunoTherapy of Cancer, conclude that this is a feasible approach for the treatment of glioblastomas. In addition, an interim survival analysis was conducted in October 2020; the results of this study will soon be available.
Although immunotherapy has become a useful treatment in cancer care, not all types of cancers are treated with it and not all tumors respond to immunotherapy. In fact, a research study published in JAMA Network Open estimated that immune checkpoint inhibitors work in only 12 percent of cancer patients eligible for treatment.
Researchers like those at Pacific Neuroscience Institute are still working on ways to improve immunotherapy so that more brain cancer patients can benefit.
About the Author

Santosh Kesari
Santosh Kesari, MD, PhD, is Director of Neuro-oncology at Pacific Neuroscience Institute and Chair and Professor, Department of Translational Neurosciences and Neurotherapeutics, Saint John’s Cancer Institute at Providence Saint John’s Health Center. He is a world leader in the innovative treatment of all types of malignant brain tumors. Dr. Kesari and his team conduct leading-edge clinical trials in immunotherapy and biomarker-based brain tumor therapies.
Last updated: January 23rd, 2021