
Brain Surgery Restores Patient’s Vision
by Amelia Garrison
Two years ago, a patient suffered sudden progressive vision loss.

When a 52-year-old woman from New York began experiencing progressive vision loss in her left eye, she knew she needed medical help. She saw an optometrist and an ophthalmologist and was quickly referred to Pacific Neuroscience Institute (PNI) after an MRI.
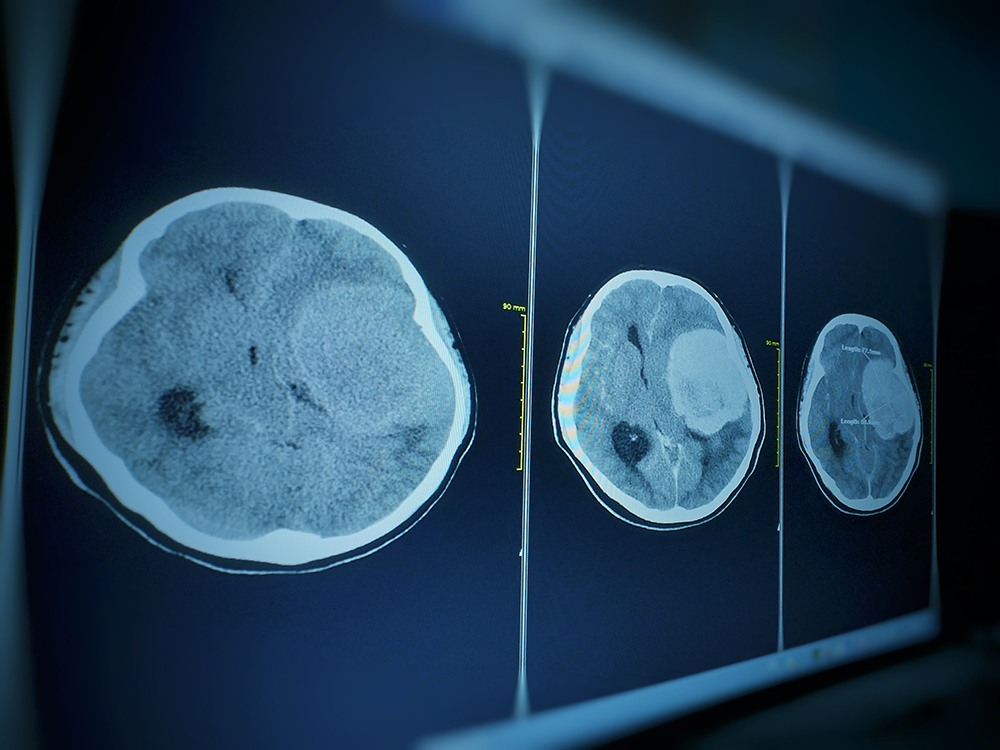
“That MRI showed an approximately two and a half by two centimeters, extra-axial brain tumor situated at the tuberculum sellae, which is a very common location for meningiomas,” explained Dr. Daniel F. Kelly, Director and one of the founders of PNI.
The Truth Behind Meningiomas
Meningiomas are categorized as benign (noncancerous) brain tumors that develop from the membrane (the “meninges”) surrounding the brain and spinal cord. They occur most commonly in people aged 40 to 70 and in women.
Although meningiomas are typically benign, they may impinge upon vital brain structures, causing disability. Symptoms may include vision loss, double vision, facial pain, difficulty swallowing, and hearing loss.
Depending on the size and location of the meningioma, symptoms may also include personality changes, seizures, motor weakness in the arms or legs, loss of sensation, spatial disorientation, and visual field deficits. This happens when a meningioma puts progressive pressure on the underlying brain.
Meningiomas are usually diagnosed incidentally by patients who receive an MRI for headaches or dizziness. First-line treatment for symptomatic meningiomas is maximal safe surgical removal. Second-line treatment is typically focused radiotherapy or radiosurgery.
Removing the Meningioma & Restoring Vision

In this particular case, the meningioma was located in the patient’s left optic canal, causing progressive vision loss. Dr. Kelly and Dr. Chester F. Griffiths, Director of the Eye, Ear & Skull Base Center and Co-Founder of PNI, used minimally invasive surgery to remove the tumor.
“Given the optic canal invasion and her primary complaint being also vision in the left eye, we approached this tumor through the endoscopic endonasal route,” recalled Dr. Kelly. “With my partner in ENT, Dr. Chester Griffiths, we were able to achieve a gross total tumor removal.”
The removal of the tumor successfully restored the patient’s vision. She recovered in two days at Providence Saint John’s Medical Center.
A Quick Recovery

At PNI, minimally invasive surgery enables patients to get out of the hospital sooner. “The goal here is to limit collateral damage to the surrounding tissues and to allow the patient to have a rapid recovery with less brain exposure, less manipulation, smaller incisions, our patients seem to have less pain,” explained Dr. Kelly.
He continued, “Our typical hospital stay for some brain tumors is one night in the hospital. Most are out by two days and rarely do they go a little bit beyond that. These [minimally invasive] approaches have multiple benefits for the patient, so we will continue to try and push the envelope on these approaches and make them even more safe and effective than they are now.”
The Follow-Up
Drs. Kelly and Griffiths have regularly checked up on the patient since her recovery two years ago.
“We have been following her now for just over two years. Her last MRI was approximately one month ago,” Dr. Kelly explained. “She’s doing great with no evidence of recurrence of the tumor and her vision is normal. And her pituitary gland function is normal and she has a normal sense of taste and smell.”
To learn more about meningioma surgery, or to get a second opinion about a newly diagnosed or recurrent meningioma, visit the meningioma page on the Pacific Brain Tumor Center.
More information: 310-582-7450
About Dr. Daniel Kelly

Daniel F. Kelly, MD, is the Director of the Pacific Brain Tumor and Pituitary Disorders Centers at Pacific Neuroscience Institute. Considered to be one of the top neurosurgeons in the U.S., Dr. Kelly is internationally recognized in the field of minimally invasive keyhole surgery for brain, pituitary, and skull base tumors. He continues to focus his efforts on advancing innovative treatments for patients, providing fellowship training in minimally invasive neurosurgery, and patient education and support.
About Dr. Chester Griffiths

Chester F. Griffiths, MD, FACS, is board certified in Otolaryngology, Head and Neck Surgery, and Facial Plastic and Reconstructive Surgery. He has 30 years of experience in endoscopic endonasal sinus surgery for skull base tumors and pituitary tumors, sinonasal cancers including mucosal melanomas, and in the treatment of facial and nasal trauma, cosmetic deformities, sinus infections, and disorders of smell and taste. His practice treats sleep apnea, snoring, difficulty breathing, disorders of the larynx, thyroid tumors, and other head and neck cancers with an emphasis on viral HPV-related cancers.
Related Links:
About the Author

Amelia Garrison
Amelia Garrison is the Marketing Specialist at Pacific Neuroscience Institute (PNI). Well versed in community outreach strategy and implementation, she leads the PNI blog, newsletter, and digital communications. Amelia oversees PNI's reputation management and community sponsorships.
Last updated: December 2nd, 2021