

Insulin Resistance and Metabolic Syndrome Implications in Parkinson’s Disease
by Melita Petrossian
In pre-clinical studies the relation of insulin resistance to the pathophysiology of Parkinson’s disease has been examined. Here we discuss the potential neuroprotective effects of diabetes medications with Parkinson’s disease.
Links Between Insulin Resistance, Metabolic Syndrome and Parkinson’s Disease
Insulin resistance (measured by elevated insulin levels or abnormal glucose tolerance test but not to the point of diabetes) and metabolic syndrome (the combination of obesity/overweight especially with increased visceral fat, prediabetes or diabetes, high blood pressure, and high cholesterol) are very common in the United States, but are also noted to have increased incidence in patients with Parkinson’s disease (PD) (Soliman et al., 2019, Kleinridders et al,. 2015). Insulin resistance may precede the development of diabetes by many years, but with treatment, diabetes can be avoided.
Growing evidence now shows an association of insulin resistance and metabolic syndrome with worse symptoms and progression of Parkinson’s disease (Papapetropoulos et al., 2004). Lima et al. (2014) have shown diabetes incidence in PD is associated with faster progression of both motor and cognitive symptoms.
Scientific Studies
In a poster presented in September 2019 at the International Congress of Parkinson’s Disease and Movement Disorders in Nice, Soliman et al. showed that insulin resistance was associated with dramatic differences in clinical symptoms and signs of patients with PD: increased tremor, rigidity, bradykinesia (slow or small movements), and postural instability, also translating as a more advanced stage of PD. Total PD scores of movement were twice as high in patients with insulin resistance than those without (where higher scores indicate worse movement). Metabolic syndrome also showed differences in motor (movement) signs and symptoms, but with less consistent effect.
For example, tremor and postural instability scores were not different, but rigidity and bradykinesia were worse in Parkinson’s disease patients with metabolic syndrome compared to without metabolic syndrome.
In addition to motor scores, cognitive differences were also noted. Attention, working memory, immediate recall, delayed recall, confrontation naming, visuoconstructional, visuospatial, alternating verbal fluency and action verbal fluency were all worse in PD patients with insulin resistance.
On scores from 0 to 134, where higher scores indicate better cognitive function, average scores in PD patients with insulin resistance were 64, compared to 99 in Parkinson’s disease patients without insulin resistance. (Though scores are from 0 to 134, normal controls have average score of 100.) Metabolic syndrome, again, showed differences, but with less dramatic effect. Attention, working memory, delayed recall, alternating verbal fluency and action verbal fluency were worse in PD patients with metabolic syndrome compared to PD patients without metabolic syndrome. Total scores were 71 versus 93 in PD patients with and without metabolic syndrome, respectively.
Multiple pre-clinical studies have examined the relation of insulin resistance to the pathophysiology of Parkinson’s disease, as well as the potential neuroprotective effects of diabetes medications such as GLP1 agonists. Considering the role of insulin resistance and metabolic syndrome as precursors of diabetes, which are more responsive to modulations in lifestyle, it seems obvious that dietary and exercise changes would be key adjuncts to the treatment of PD.
The above-mentioned study is limited by potential confounders such as vascular disease (stroke) and neuropathy, for which patients with insulin resistance and metabolic syndrome may be at higher risk, and which may worsen PD-related motor and cognitive signs. Also, both insulin resistance and metabolic syndrome may be seen more commonly in sedentary patients, and there are other (non-insulin-mediated) mechanisms by which exercise (or lack thereof) may play a role in Parkinson’s disease motor and cognitive symptoms.
Insulin Resistance Management
That being said, regardless of the mechanism, it seems clear that there are multiple reasons to assess and manage insulin resistance and metabolic syndrome. Exercise, weight loss, low calorie and reducing sugar in the diet can reduce the risk of insulin resistance and metabolic syndrome. In addition, sleep quality plays a role in the development of metabolic syndrome so a management strategy may include assessing for underlying sleep apnea and/or improving sleep quality and quantity.
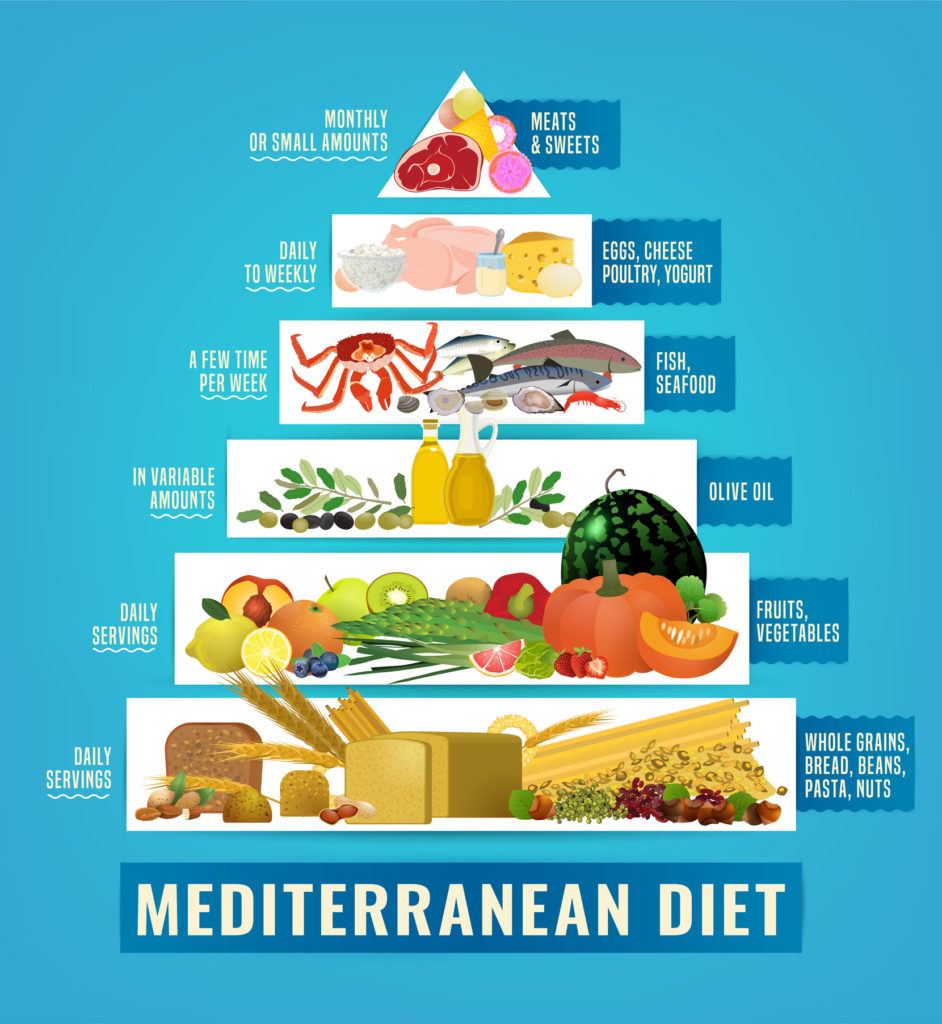
As far as dietary management of insulin resistance, a key point is the amount and type of carbohydrate intake. Excess (added) sugar, highly processed foods, and high glycemic index foods should be avoided. Examples include sweets, white bread, white rice, fruit juice, table sugar, potato-based foods and corn-based foods. Lower glycemic index carbohydrates, such as brown rice and whole grain breads, non-starchy vegetables such as beans, carrots, greens, etc., have higher fiber and lower the risk of insulin resistance. The Mediterranean diet has consistently been shown to lower the risk of metabolic syndrome and insulin resistance.
Conclusion
Further studies on diabetes medications are necessary and underway, especially regarding GLP1 agonists, to further reduce the progression of PD, after the publishing of a promising trial on exenatide showing reduced motor progression compared to placebo (Athauda et al., 2017).
I feel the results of this small study were dramatic and I hope PD patients feel empowered to minimize PD symptoms and progression by addressing lifestyle factors that can contribute to insulin resistance and the metabolic syndrome.
About the Author

Melita Petrossian
Melita Petrossian, MD, is Director of Pacific Movement Disorders Center and is a fellowship-trained neurologist with clinical interests and expertise in movement disorders such as Parkinson’s disease, essential tremor, dystonia, gait disorders, ataxia, myoclonus, blepharospasm, hemifacial spasm, Meige syndrome, spasticity, tics, and Tourette’s syndrome. She also specializes in Parkinson’s-related conditions such as Dementia with Lewy Bodies, progressive supranuclear palsy, multiple system atrophy, corticobasal degeneration, primary freezing of gait, and Parkinson’s disease dementia.
Last updated: March 23rd, 2020