

PNI Scientists Explore Using Psychedelics to Treat Alcohol, Drug Disorders
by Guest Author
Psilocybin and many other psychedelics are broadly prohibited under federal law. But US researchers at PNI’s Pacific Treatment & Research In Psychedelics (TRIP) program have been legally scrutinizing their use in a score of clinical trials. Read the latest feature of the TRIP program in the Los Angeles Times.
Melanie Senn’s father, long dead, appeared to her as she lay back in the dimly lit room at the Santa Monica clinic, a mask over her closed eyes, and the psychedelic trip began.
More precisely, it was his thumb. It was disembodied and huge, materializing in her mind to wipe away her own image. Just as a parent might lick a thumb, she said, and use it to clean the dirtied cheek of a child.
“It wasn’t like an aggressive move,” said Senn, 51, recounting the experience. Her father’s thumb had appeared right after the word “goodbye” stretched before her, like a banner in the sky.
“It was like, ‘Goodbye. We’re going somewhere else. And you cannot take this version of yourself,’” she recalled.
Her father had died decades earlier after struggling with alcohol use disorder and bouts of homelessness. She didn’t see herself as an alcoholic — it was a word that seemed out of place in her stable life as an educator, wife and mother — but she had begun to think about how much wine she was drinking at night, the sapped energy and headaches she endured by day.
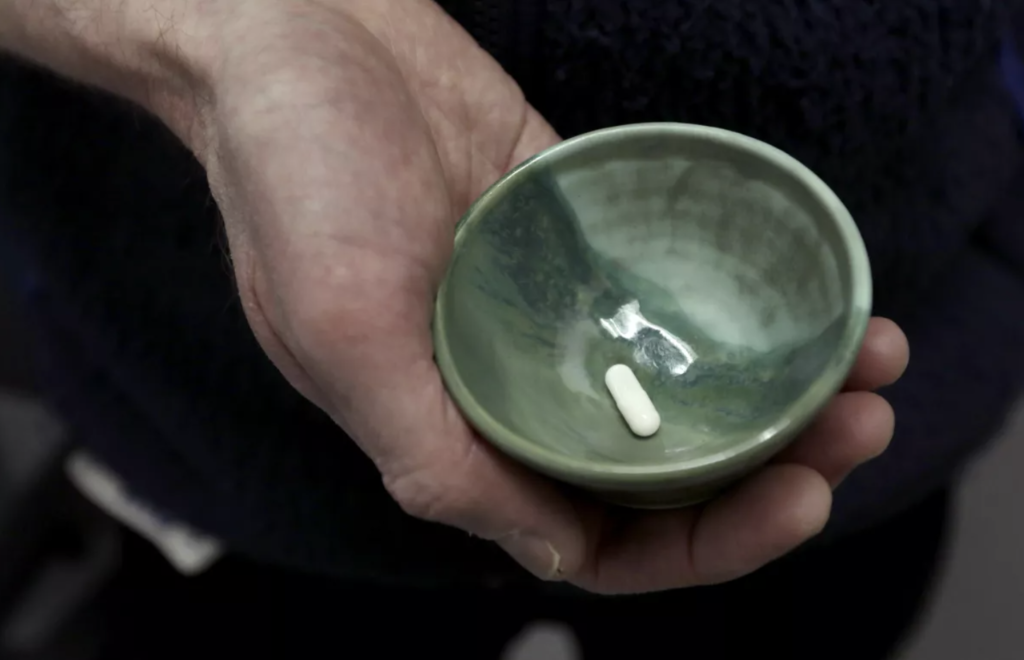
Senn, who lives in San Luis Obispo, said she had signed up for the clinical trial, hours away in Santa Monica, to see whether therapy with psilocybin, the chemical compound in “magic mushrooms” that can cause hallucinations, might change her relationship to a much more familiar and socially sanctioned drug.
“If my dad had had access to psilocybin treatment,” she had wondered before her trip at the Pacific Neuroscience Institute® (PNI) “could that have helped him?”
Psilocybin and many other psychedelics are broadly prohibited under federal law, and categorized by the Drug Enforcement Administration as having “no currently accepted medical use.”
Yet US researchers have been legally scrutinizing possible uses of psychedelics in scores of clinical trials approved by the government, addressing their effects on anorexia, migraines, and a range of other maladies.
The Food and Drug Administration has deemed psilocybin a potential “breakthrough therapy” for treating depression, a designation that could fast-track the path to new pharmaceuticals.
Popular interest in psychedelics has been bolstered by the books of Michael Pollan, whose writing inspired Senn to look up psilocybin trials. And money, long the limiting factor in psychedelic research, is pouring into the field from corporate investors and intrigued philanthropists.
Addiction treatment has been one of the most keenly watched areas of psychedelics research in recent years, as studies explore whether they could help people shake off the need for other substances, both legal and illegal.
Early studies have shown promise in treating addiction to tobacco and alcohol. The question has gained urgency as the US faces an overdose surge that is killing more than 100,000 people annually, the majority linked to opioids, and a spike in deaths tied directly to alcohol, which have hit their highest rate in decades.
At Johns Hopkins University, researchers examining whether psilocybin could help with tobacco cravings received a grant in 2021 from the National Institutes of Health — the first the agency has awarded in more than half a century to study therapeutic uses of a psychedelic drug.
Physicians in New York and New Mexico published a study this summer finding that patients treated with psilocybin and psychotherapy cut back more on heavy drinking than those who received psychotherapy and a placebo.
Researchers are exploring possible benefits for cocaine users. Others have hoped to turn the powers of psychedelics toward easing opioid addiction.
Experts say it’s unclear exactly why psychedelics seem to help some people with addiction.
Scientists have found that psilocybin acts on key areas of the brain that are important in addiction. Psilocybin also indirectly stimulates a receptor for serotonin, a chemical in the brain that plays a role in addictive behavior.
Some researchers say a psychedelic trip appears to free the brain to make new connections and eject itself from familiar ruts — a tool that could help patients break loose from destructive ways of thinking.

(Genaro Molina / Los Angeles Times)
However, research on psychedelics is in its early stages. It’s unclear whether the hallucinations tied to psilocybin are critical to any therapeutic effects or could be disentangled from them in a new medication. Psychedelic research has also struggled to find a placebo that participants cannot easily distinguish from a psychedelic trip.
Psychedelics have known risks, especially outside a clinical setting where patients are being monitored, experts have warned.
People undergoing psychedelic trips may see things that are disturbing, experience increases in heart rate or blood pressure, panic, and put themselves in danger or be vulnerable to exploitation. In rare cases, users may suffer ongoing problems such as paranoia or hallucinatory flashbacks, according to the National Institute on Drug Abuse.
As scientists probe possible benefits in therapy, some local laws on psychedelics have been eased.
In Oregon, voters passed measures to create a regulatory framework for the use of psilocybin in supervised settings and eliminate criminal penalties for possessing limited amounts of controlled substances, including psilocybin and many other psychedelics. Colorado voters in November passed a measure to decriminalize the personal possession of psilocybin and other psychedelic plants.
In 2022, California lawmakers weighed a bill proposed by state Sen. Scott Wiener (D-San Francisco) that would have allowed the possession of psilocybin and several other hallucinogenic drugs for personal or facilitated use. Among those lobbying for the California bill were military veterans who say psychedelic treatment helped them with addiction and trauma.
Opponents of the California bill contended that therapeutic uses should not be conflated with decriminalizing such drugs more broadly. The group Crime Victims United of California argued that a possible therapeutic benefit “by no means justifies their wholesale legalization for the masses — who are not necessarily under the watchful eye of a licensed therapist.”
The bill was scaled back to a proposed study, then shelved in the fall. Wiener pledged to try again and recently introduced a revised version of the proposal.
In Santa Monica, TRIP Program Director Keith Heinzerling, MD has long wondered about those crucial moments that people talk about in Alcoholics Anonymous.
“They talk about these epiphanies, where the switch flips and then they just feel different,” said Dr. Heinzerling, who was an addiction-medicine doctor and researcher at UCLA before joining the Pacific Neuroscience Institute. “Myself and some of the clinicians were always like, ‘How do you facilitate that?’ Because people would try, try, try — and it would happen at the least expected time.”
Psychedelics seem to him like one way to help patients get to those transformative moments — “a roller coaster that takes you on a tour of your inner self.” Heinzerling describes psychedelics as the most empowering model for therapy he has found.
“It’s not mind control,” he said. “It’s a door that you can choose to open.”
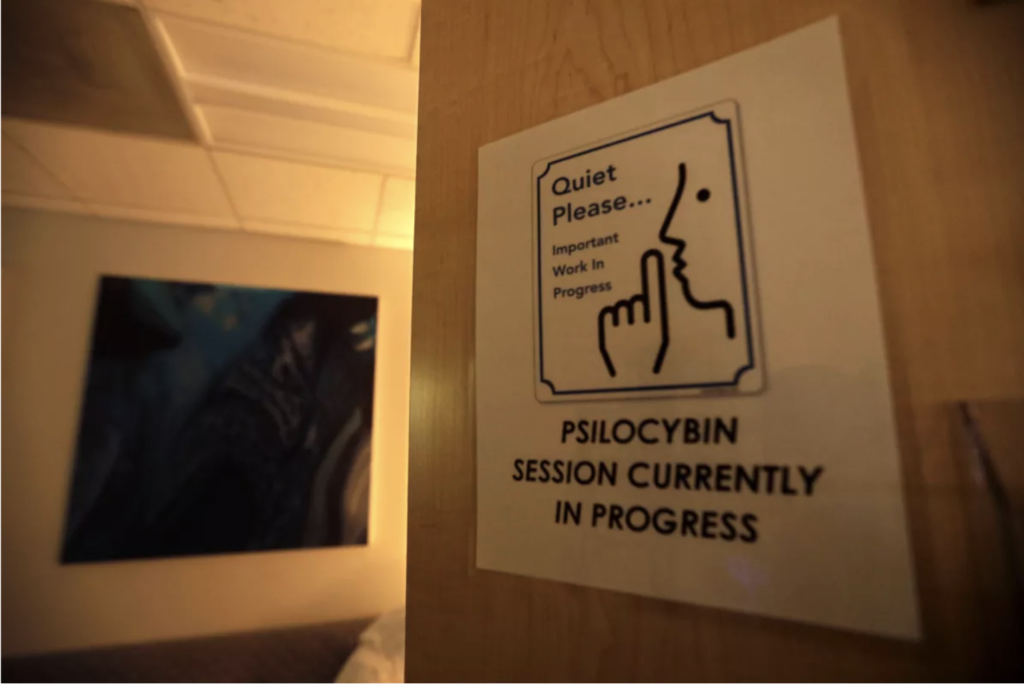
The Treatment & Research In Psychedelics program — better known as TRIP — has let patients, through federally regulated clinical trials, open that door in a softly lit room with a comfortable sofa and attentive therapists.
One of the latest studies, which recruited participants with alcohol use disorder, sought to gauge the safety and tolerability of playing a video — with classical music trickling over majestic scenes of butterfly wings, mountain ridges, and waterfalls — to ease patients into the experience before they cover their eyes.
Heinzerling said the therapists reassure participants that “we’re going to keep your body safe here — and allow you to let your mind go.” After the psilocybin session, they meet again weekly through the course of the study to talk about the experience, with therapists helping patients process what they felt and saw.
Senn, one of a score of people participating in that pilot study, called it “hands-down the most profound experience of my life.” During her trip, she said, she experienced her father gently wiping away her image — “almost like he was erasing my ego” — then taking her to a celestial place that she strained to describe in words.
“I’m not a religious person,” she said, “but I truly think I have now been cured of my atheism.”
At one point, she saw her own children, connected to her with long, black umbilical cords; at another, she opened her mouth, and incandescent light poured out of her like a bulb as the message “No one is angry at you” resounded. She saw her mother, shrouded in a dark covering of wraiths, bones, and melting faces, and felt her overwhelming grief.
“I felt completely wrung out afterward,” she said. “Kind of just raw, but also, like, soft and in awe.” A friend picked her up from the Santa Monica clinic and drew her a bath, where she soaked for hours.
Her husband joked on the phone, “Are you coming back a teetotaling vegan?” This was, after all, a study related to alcohol that required her to track how many drinks she had each day.
Senn said the depth of her psychedelic experience feels at odds with making simple declarations like “I’m not going to drink anymore.” But tripping through the cosmos with her long-deceased father did bring home to her that “you have all these connections. You have all this love. … You don’t have to hurt yourself.”
Months after taking psilocybin, she drank less, then not at all. Senn said her psychedelic trips were one part of a bigger journey that included changing her career, reading books on addiction, meditating, writing, and practicing yoga. The transcendent beauty of her experience, she said, had made drinking seem dull and limiting.
“Seeing this sublime connection is making me feel so alive,” she said. “So much more alive than drinking myself to sleep.”
More information:
Ketamine Treatment: 310-582-7612 | Clinical Trials: 310-582-7611
About Dr. Keith Heinzerling

Keith Heinzerling, MD, practices internal medicine and is an addiction medicine specialist at the Pacific Brain Health Center, Pacific Neuroscience Institute. His clinical and research focuses are on the treatment of alcohol, drug and substance use problems, with anti-addiction medications. As director of the Treatment & Research In Psychedelics (TRIP) program, he is involved in the development of psychedelic-assisted therapies for those suffering with addiction, depression, anxiety, and PTSD.
Useful Links
- Treatment & Research In Psychedelics (TRIP)
- Anxiety Research Study
- Ketamine Assisted Therapy Program
 Psychedelic-Assisted Therapy with Ketamine at PNI
Using ketamine in a psychedelic-assisted approach, we treat people 16 years and older who are treatment-resistant or who wish to effectively tackle deep-rooted, unresolved trauma that has not been adequately…
Psychedelic-Assisted Therapy with Ketamine at PNI
Using ketamine in a psychedelic-assisted approach, we treat people 16 years and older who are treatment-resistant or who wish to effectively tackle deep-rooted, unresolved trauma that has not been adequately…
 Think Neuro Podcast: The Promise of Psychedelics | Dr. Keith Heinzerling & Louie Schwartzberg
Addiction and depression are two of the most widespread conditions in all of medicine. After decades of research, doctors are still looking for alternatives for when medication and cognitive training…
Think Neuro Podcast: The Promise of Psychedelics | Dr. Keith Heinzerling & Louie Schwartzberg
Addiction and depression are two of the most widespread conditions in all of medicine. After decades of research, doctors are still looking for alternatives for when medication and cognitive training…
 Meet Dr. Heinzerling
Dr. Heinzerling is the Director, Pacific Treatment & Research In Psychedelics Program; Internal Medicine – Addiction Medicine, Brain Health Center. He practices internal medicine and is an addiction medicine specialist…
Meet Dr. Heinzerling
Dr. Heinzerling is the Director, Pacific Treatment & Research In Psychedelics Program; Internal Medicine – Addiction Medicine, Brain Health Center. He practices internal medicine and is an addiction medicine specialist…
 Psychedelic-Assisted Therapy at Pacific Neuroscience Institute
Dr. Keith Heinzerling is an addiction medicine specialist and Director of Treatment & Research In Psychedelics (TRIP) at Pacific Neuroscience Institute in Santa Monica, CA. Learn about how psychedelic-assisted therapy…
Psychedelic-Assisted Therapy at Pacific Neuroscience Institute
Dr. Keith Heinzerling is an addiction medicine specialist and Director of Treatment & Research In Psychedelics (TRIP) at Pacific Neuroscience Institute in Santa Monica, CA. Learn about how psychedelic-assisted therapy…

Psychedelic-Assisted Therapy with Ketamine at PNI

The Promise of Psychedelics | Dr. Keith Heinzerling & Louie Schwartzberg

Meet Dr. Heinzerling
Psychedelic-Assisted Therapy at Pacific Neuroscience Institute
Last updated: January 10th, 2023