
4 Factors for Successful Deep Brain Stimulation in Movement Disorders
by Jean-Philippe Langevin
Getting the Best Results from Deep Brain Stimulation Surgery
Deep brain stimulation (DBS) surgery can improve the quality of life of patients suffering from various movement disorders including Parkinson’s disease, essential tremor and dystonia. Undergoing surgery is an important and personal decision in the patient’s life and ultimately, most potential candidates consider the likelihood of meaningful benefit against the risks of surgery. The response from DBS can vary from patient to patient, however a multidisciplinary team approach can often optimize the results from surgery. Our specialized medical team considers and discusses four main factors:
1. Confirming that the diagnosis is accurate
2. Selecting the appropriate brain target for optimal benefit
3. Precisely placing electrodes using a customized guidance system such as a mini frame
4. Device programming and post-operative long-term management
Pre-operative Evaluation
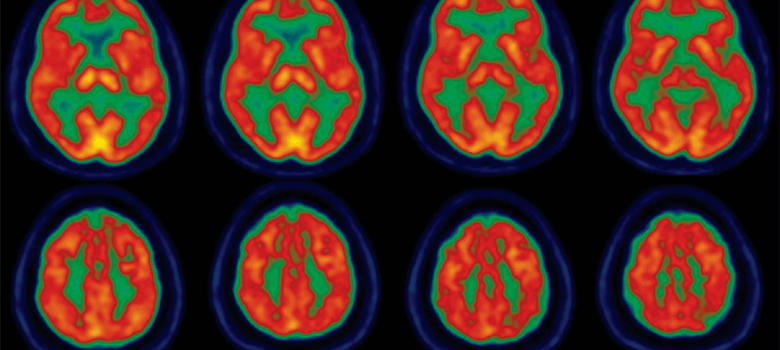
A successful surgery starts even before the decision to operate is made. Determining the accurate diagnosis is especially critical for optimal surgical outcomes. For instance, implanting DBS electrodes for a patient suffering from a syndrome mimicking a movement disorder will provide little or no benefit. This is highlighted in our article published in the November 2016 issue of Surgical Neurology International: Stereotactic Supplement – Deep brain stimulation of a patient with psychogenic movement disorder. The patient previously diagnosed with Parkinson’s disease presented to us after being treated with DBS for five years but without any significant symptom improvement. Our evaluation revealed that the patient was not suffering from Parkinson’s disease and a normal DaTscan supported this conclusion.
 The DaTscan is a nuclear medicine imaging test that specifically targets the dopamine transporter (DaT). That transporter pumps dopamine back into neurons so that it can be reused for the next signal transmission allowing normal movement. DaT increases the overall amount of dopamine available for neurotransmission. With Parkinson’s disease, neuronal loss leads to a reduction in DaT, which is detected by the scan in patients presenting with tremors and other symptoms associated with this movement disorder. Further psychiatric and neurological evaluations revealed that the patient was suffering from a psychogenic movement disorder, that is, the symptoms had a psychological origin or cause rather than a physical one.
The DaTscan is a nuclear medicine imaging test that specifically targets the dopamine transporter (DaT). That transporter pumps dopamine back into neurons so that it can be reused for the next signal transmission allowing normal movement. DaT increases the overall amount of dopamine available for neurotransmission. With Parkinson’s disease, neuronal loss leads to a reduction in DaT, which is detected by the scan in patients presenting with tremors and other symptoms associated with this movement disorder. Further psychiatric and neurological evaluations revealed that the patient was suffering from a psychogenic movement disorder, that is, the symptoms had a psychological origin or cause rather than a physical one.
This experience illustrates the safety of DBS where the patient did not suffer from any side effects despite receiving several years of continuous therapy while in fact, not suffering from a neurological movement disorder at all. This suggests that DBS does not impose long term changes to the brain circuits and more importantly, this clinical vignette shows the importance of an accurate diagnosis. An expert movement disorders neurologist is essential to conduct an accurate evaluation taking into account patient history, physical condition and the prior clinical response. For Parkinson’s disease, an important indicator is a positive response to dopamine medication such as L-Dopa while adjunct tests, such as the DaTscan, available at Providence Saint John’s Health Center, may also assist with the diagnosis. However, the experience of the clinician remains critical.

The advantage of a team approach is well exemplified when selecting the brain target for a specific patient. This decision can require input from the movement disorder neurologist, the neurosurgeon and the neuropsychologist. With a comprehensive approach, the team can consider the unique presentation of the patient including the specific symptoms causing the disability, the precise anatomy of the brain and finally the psychological and cognitive state. These factors are important to take into account when selecting the best target to improve the symptoms without altering the patient’s psychological state.
The Surgery

Several technical advancements have improved the precision of electrode placement in recent years. Conventional stereotactic fixed frames remain very reliable, and as with other medical machinery, they require maintenance and verification to insure accuracy. Newer technologies focus on individualization of care. For instance, a custom-made mini frame from FHC, is created specifically for a patient, is used only once and allows bilateral electrode insertion simultaneously. Furthermore, the device is significantly lighter than a conventional frame and does not require head fixation during the surgery. Finally, very few or no measurements are required during the procedure as the mini frame has already been tailored for a specific patient so that the surgery becomes more comfortable and shorter in duration. Comfort during surgery can also improve accuracy because it permits a more thorough testing of the electrodes intra-operatively to determine if the optimal placement is achieved while shorter procedure time is highly desirable for reducing certain operative risks.
Accurately inserting the electrode at a predetermined location is not the only determinant of precise placement. In order to stimulate the right location, it is equally important to understand the local anatomy of a specific patient. The classical technique for electrode placement involves the use of surgical coordinates based on historical atlases. This approach assumes that structures are approximately in the same location from patient to patient. Our more individualized strategy takes advantage of refined MRI sequences that delineate the target region. In this case, the electrode is inserted in the appropriate region through direct visualization of a specific anatomical target.
Post-operative Evaluation
 In addition, the success of DBS surgery depends on the quality of the care after the procedure. Optimal post-operative management and device programming is best performed through a multidisciplinary approach. The accurate electrode location in relation to the patient’s anatomy along with the symptoms to be treated are considered. Post-operative imaging can be used to determine the position of the electrode in the target region allowing for accurate stimulation. The patient’s medication should also be adjusted as the DBS system is programmed and the medication can often be reduced slightly once DBS is initiated.
In addition, the success of DBS surgery depends on the quality of the care after the procedure. Optimal post-operative management and device programming is best performed through a multidisciplinary approach. The accurate electrode location in relation to the patient’s anatomy along with the symptoms to be treated are considered. Post-operative imaging can be used to determine the position of the electrode in the target region allowing for accurate stimulation. The patient’s medication should also be adjusted as the DBS system is programmed and the medication can often be reduced slightly once DBS is initiated.
In conclusion, a successful DBS surgery starts in the planning phase prior to the procedure itself and it continues well beyond the device implant. Along all those steps, an experienced multidisciplinary team can help make decisions based on the need of individual patients. Personalization of care is important and should be followed throughout the therapy in order to improve the chance of a positive outcome. Several decisions should be tailored for every patient. In particular, the specific symptoms causing the disability alongside the baseline psychosocial state of the patient have to be considered when determining the best DBS target. In addition, imaging sequences now permit direct visualization of the patient’s anatomy so that generalization based on atlases is no longer necessary. Finally, new technologies such as custom-made mini frames bring individualized of care to the operating room, therefore improving comfort and reducing surgical time.
For more information about Deep Brain Stimulation or for a consultation, please contact Pacific Movement Disorders Center at 310-582-7433.
Dr. Jean-Philippe Langevin is a board-certified and fellowship-trained neurosurgeon specializing in the surgical treatment of movement disorders, epilepsy and psychiatric conditions. As Director of the Restorative Neurosurgery and Deep Brain Stimulation at the Pacific Movement Disorders Center, he has extensive experience using neuromodulation to treat conditions such as Parkinson’s disease, essential tremor, dystonia, epilepsy and obsessive-compulsive disorder (OCD). He employs a variety of treatment modalities including deep brain stimulation (DBS), vagal nerve stimulation (VNS) and interstitial laser ablation.
Dr. Melita Petrossian is Director of Pacific Movement Disorders Center and is a fellowship-trained neurologist with clinical interests and expertise in movement disorders such as Parkinson’s disease, essential tremor, dystonia, gait disorders, ataxia, myoclonus, blepharospasm, hemifacial spasm, Meige syndrome, spasticity, tics, and Tourette’s syndrome. She also specializes in Parkinson’s-related conditions such as Dementia with Lewy Bodies, progressive supranuclear palsy, multiple system atrophy, corticobasal degeneration, primary freezing of gait, and Parkinson’s disease dementia.
About the Author

Jean-Philippe Langevin
Dr. Jean-Philippe Langevin is a board-certified and fellowship-trained neurosurgeon specializing in the surgical treatment of movement disorders, epilepsy and psychiatric conditions. As Director of the Restorative Neurosurgery and Deep Brain Stimulation at the Pacific Movement Disorders Center, he has extensive experience using neuromodulation to treat conditions such as Parkinson’s disease, essential tremor, dystonia, epilepsy and obsessive-compulsive disorder (OCD). He employs a variety of treatment modalities including deep brain stimulation (DBS), vagal nerve stimulation (VNS) and interstitial laser ablation.
Last updated: August 2nd, 2019