
Glioblastoma Awareness Day: Confronting the Challenges of a Devastating Brain Tumor
by Brianna Rauchman
Today, July 19, 2023, marks the observance of Glioblastoma Awareness Day. Glioblastoma (GBM) is an infamous form of brain cancer, presenting immense difficulties in its treatment. Notably, it garnered significant attention in the past years due to the unfortunate loss of notable political figures like Beau Biden, Ted Kennedy, and John McCain, all succumbing shortly after diagnosis.
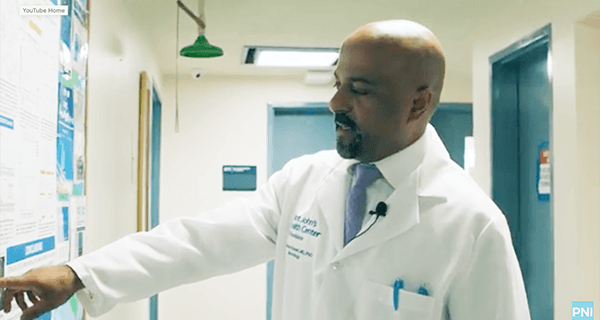
In this article, we sat down with Santosh Kesari, MD, PhD, acclaimed neuro-oncologist and a co-founder of Pacific Neuroscience Institute, and Akanksha Sharma, MD, board-certified neurologist and neuro-oncologist, to discuss this complex disease.
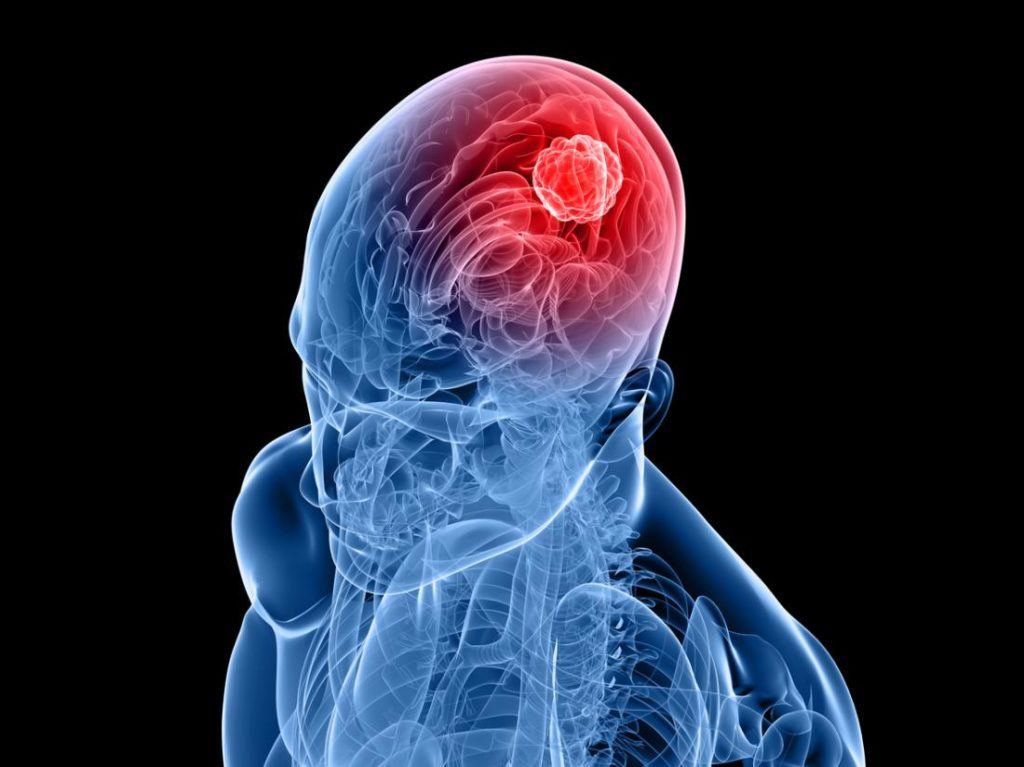
What is glioblastoma?
Types of GBM
According to Dr. Kesari, “There are two types of glioblastomas: primary, originating de novo, and secondary, evolving from lower-grade gliomas.” Patients diagnosed with these tumors generally have a dismal prognosis and poor quality of life as the disease progresses. In the United States, an estimated 13,000 patients are diagnosed with GBM annually, with a life expectancy of about 14 months, and a 5-year survival rate of 5%. The incidence increases dramatically after the age of 54 years and reaches a peak incidence at age 75-84 years.
Symptoms of GBM
“One of the most common symptoms is a headache, which differs from a typical tension or migraine headache. Other symptoms which may occur alone or in combination include persistent weakness, numbness, blurred vision, balance issues, seizure, changes in memory, or alteration of language,” reveals Dr. Kesari.
“In a vast majority of patients, there is no cause of the disease, but we presume there is an initial molecular event in a cell that starts to become cancerous,” Dr. Kesari adds. The only well-established causative factor for GBM is exposure to ionizing radiation, but this accounts for only a small minority of cranial tumors. Currently, MRI imaging provides the most sensitive tool for the initial detection of GBM; however once a GBM is identified, the tumor is already at an advanced state.
The standard of care therapy consists of debulking surgery, followed by radiation and temozolomide chemotherapy. The radiation and chemotherapy agent damages the DNA in tumor cells that are actively dividing.
Why is glioblastoma difficult to treat?
- Heterogeneity: There is a high degree of variation (heterogeneity) within the same tumor cells that makes each individual glioblastoma molecularly distinct. This can be challenging when predicting prognosis and treatment
- Location of tumor: If the tumor is located in a region that is hard to reach, or too near vital blood vessels or crucial brain regions, it can render surgery high-risk or impossible.
- Recurrence: GBM tumors have a tendency to come back aggressively.
Dr. Kesari explains that the challenge in treating brain tumors lies in addressing inactive tumor cells, which are dormant. These cells, known as cancer stem cells, evade radiation and chemotherapy by remaining inactive.
Coping with a Glioblastoma Diagnosis
Few cancers are as challenging as glioblastomas. Although no cure currently exists for these brain tumors, patients and care partners can take steps to enhance their quality of life after receiving a diagnosis. Fortunately, Dr. Sharma possesses extensive knowledge in this area.
Everything happens very fast, and it’s very overwhelming, so you are fine one day, you have a seizure and a big mass in your head. You’re being rushed into surgery…There is so much information, so many different things to consider.
Dr. Sharma
As a specialist in palliative medicine, her objective is to create an open and safe environment where patients can engage in meaningful conversations and candid dialogues with their loved ones. Her goal is for patients to cherish and create new memories while maximizing their time. Furthermore, Dr. Sharma strives to align treatment with patient goals and provide comprehensive care, which encompasses thorough symptom assessment and management, as well as support for the patient’s family and friends.
Clinical Trials and Research for Glioblastoma
Dr. Kesari has significantly advanced the fight against glioblastoma by developing treatment methods that target and destroy cancer stem cells. Recently, he successfully completed a phase 2 clinical trial using an immunotoxin, which demonstrated promising results.
There is a need for better therapies in brain cancer patients, and by studying the molecular genetic of patients, I believe we are on the verge of getting there. Many of these challenges are currently being studied in clinical trials and by having an understanding of glioblastoma we hope to soon have a cure.
Dr. Kesari
Currently, there are several active clinical trials being conducted at Saint John’s Cancer Institute and Pacific Neuroscience Institute. These are new treatment approaches for those who are newly diagnosed with glioblastoma, and those who have recurrent disease.

One of Dr. Kesari’s main objectives is to help cancer patients gain access to promising clinical trials based on thorough research and evaluation of published data. Having personal experience with treatments such as immunotherapy, which modifies the immune system to recognize and combat cancerous cells, as well as precise therapeutic approaches that focus on brain tumors at the molecular level, he holds the belief that there is hope in the battle against GBM. Learn more about Pacific Brain Tumor Center clinical trials and research.
GBM Awareness Day 2023
July 19 marks Glioblastoma Awareness Day in the United States. The aim is to honor those who battled glioblastoma and showcase the fortitude of patients and caregivers. Additionally, we must acknowledge the tireless efforts of medical professionals and researchers in seeking a cure.
For GBM Awareness Day, Dr. Kesari encourages using the #GBMAwareness hashtag to amplify the need for increased research funding. Furthermore, Dr. Sharma, along with care partners Art Krueger and Kathy Savits, reveal the challenges of GBM, and convey solidarity to patients and care partners in a new video with the National Brain Tumor Society.
Relevant Links
- Pacific Brain Tumor Center
- Glioma & Glioblastoma
- Glioma & Glioblastoma Treatment
- Research & Clinical Trials
About Dr. Santosh Kesari

Neuro-oncologist Dr. Santosh Kesari, MD, PhD, is a board-certified neurologist and is currently Chair and Professor, Department of Translational Neurosciences, Saint John’s Cancer Institute. He is the regional medical director of Providence Southern California’s Research Clinical Institute. Dr. Kesari is also Director of Neuro-oncology at Pacific Neuroscience Institute, Providence Saint John’s Health Center, and Providence Little Company of Mary Medical Center Torrance, and leads the Pacific Neuroscience Research Center at Pacific Neuroscience Institute.
About Dr. Akanksha Sharma

Akanksha Sharma, MD, is board certified in neurology, neuro-oncology and palliative medicine. She is experienced in the treatment of primary/metastatic brain tumors, neurological complications of cancer, and disease-related burden and symptoms. Her clinical and research interests lie in helping patients maximize their time and quality of life. She aims to align treatment with patient goals and to provide holistic care that includes careful symptom assessment and management, as well as support for the patient’s loved ones.
Related Articles
Related Videos
 Glioblastoma Clinical Trial with Phase One Foundation | Santosh Kesari, MD, PhD
PHASE ONE Foundation provided the initial funding for a breakthrough clinical trial for patients with brain cancer. The trial’s principal investigator and author Santosh Kesari, MD, PhD, conducts the study…
Glioblastoma Clinical Trial with Phase One Foundation | Santosh Kesari, MD, PhD
PHASE ONE Foundation provided the initial funding for a breakthrough clinical trial for patients with brain cancer. The trial’s principal investigator and author Santosh Kesari, MD, PhD, conducts the study…
 Coping with a Glioblastoma Diagnosis | Dr. Akanksha Sharma & Maria Quiban Whitesell
There are few cancers more challenging than glioblastomas. While there is currently no cure for these brain tumors, patients and their caregivers can take steps to maximize their quality of…
Coping with a Glioblastoma Diagnosis | Dr. Akanksha Sharma & Maria Quiban Whitesell
There are few cancers more challenging than glioblastomas. While there is currently no cure for these brain tumors, patients and their caregivers can take steps to maximize their quality of…
 Brain Tumor Webinar: Living with Optune (Tumor Treating Fields) for Glioblastoma
Guest Speaker Janice discusses what is it like to live with Optune (Tumor Treating Fields) for glioblastoma. The webinar was hosted by Akanksha Sharma, MD, Neuro-oncologist at the Pacific Brain…
Brain Tumor Webinar: Living with Optune (Tumor Treating Fields) for Glioblastoma
Guest Speaker Janice discusses what is it like to live with Optune (Tumor Treating Fields) for glioblastoma. The webinar was hosted by Akanksha Sharma, MD, Neuro-oncologist at the Pacific Brain…
 Frank’s Story – Glioblastoma
Experience an actual account of Glioblastoma.
Frank’s Story – Glioblastoma
Experience an actual account of Glioblastoma.
 Rusty’s Story – Glioblastoma
Rusty’s Glioblastoma journey and the Pioneers of Innovation behind the MDNA55 clinical trial.
Rusty’s Story – Glioblastoma
Rusty’s Glioblastoma journey and the Pioneers of Innovation behind the MDNA55 clinical trial.
Glioblastoma Clinical Trial with Phase One Foundation | Santosh Kesari, MD, PhD
Coping with a Glioblastoma Diagnosis | Dr. Akanksha Sharma & Maria Quiban Whitesell

Brain Tumor Webinar: Living with Optune (Tumor Treating Fields) for Glioblastoma
Frank’s Story | Glioblastoma

Rusty’s Story
About the Author
Brianna Rauchman
Brianna Rauchman, BA, is the Communications Coordinator for the Lifestyle Program, where she helps develop outreach strategies to connect with an expanding audience. Her responsibilities include providing launch support, developing content, assisting with collateral design, and planning social media strategies.
Last updated: July 20th, 2023



