

Brain Surgery Through the Eyebrow
by Daniel F. Kelly
An excellent team of outstanding neurosurgeons at Pacific Neuroscience Institute’s Brain Tumor Center has reported on 129 minimally invasive supraorbital (SO) surgeries in a recent paper; the highly encouraging results of a retrospective study are discussed.
Minimally Invasive Surgery for Removal of Brain and Skull Base Tumors
Neurosurgeons have been exploring the possibility of less invasive craniotomy to access intracranial tumors for over 50 years.
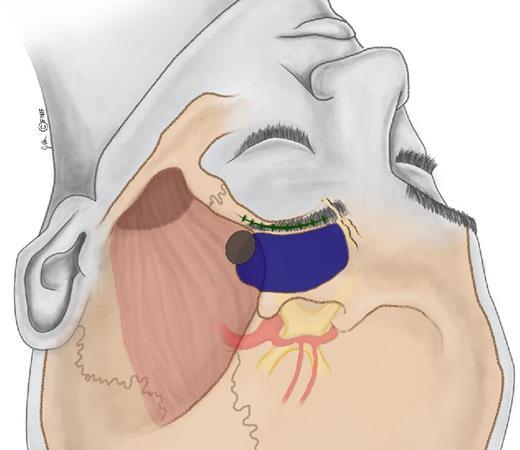
The benefits of minimally invasive surgical techniques to remove brain tumors potentially include faster recovery, and less damage to the surrounding brain structures. Various minimally invasive surgeries include, endonasal (via the nostrils), supraorbital (through the eyebrow), retro-mastoid (behind the ear), and gravity-assisted approaches.
The PNI neurosurgical and ENT team has a long track record in performing and enhancing these minimally invasive approaches to make them safer and more effective. This paper is another example of the innovative care provided for patients with brain, pituitary and skull base tumors at PNI.
What is eyebrow (supraorbital) craniotomy?
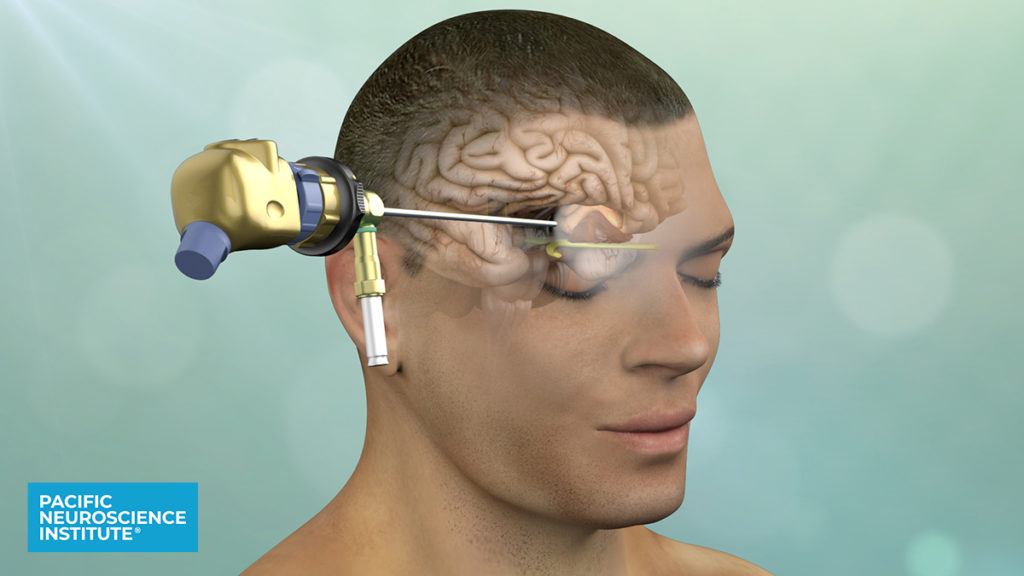
Eyebrow craniotomy (supraorbital, SO) is a minimally invasive surgical procedure that is used for the removal of certain brain tumors located in or under the frontal lobes and around the area of the optic nerves and above the pituitary gland. An incision in the eyebrow allows access to frontal regions of the brain followed by microsurgical removal of the tumor; in most cases, a high-definition endoscope is also used for enhanced visualization to allow maximal safe tumor removal by providing a better view of tumor that may not be directly visible to the surgeon with the operating microscope alone. For surgery, the patient is placed such that the eyebrow is easily accessible by the neurosurgical team.
The eyebrow incision procedure was developed in the 1990s and early 2000s and has clear advantages over traditional invasive surgery. Not only does it significantly decrease brain exposure, it also reduces scalp and muscle manipulation, the need for brain retraction, and in most cases, has an excellent aesthetic outcome.
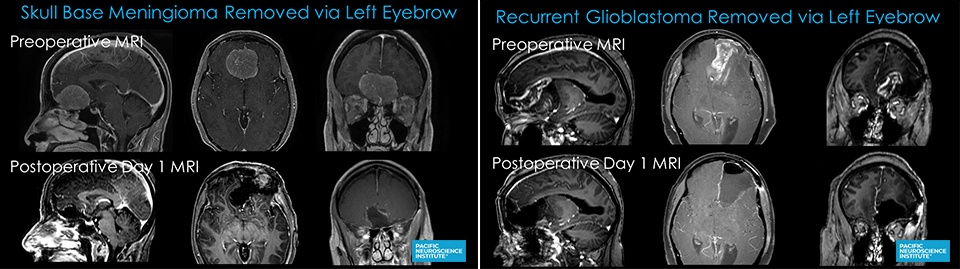
It is especially effective for the removal of meningiomas, gliomas and metastases, and the success rate is further increased when used in conjunction with endoscopy.
The supraorbital eyebrow craniotomy, when performed by experienced surgical teams has proved to be a versatile, safe and effective procedure for many tumor types, promoting a more rapid recovery and a return to more normal lifestyle.
A retrospective study
In a recent study by Ansari et al1, data was analyzed from 129 SO surgeries conducted on 117 patients between 2007 and 2018. In particular, two parameters were evaluated:
- The effectiveness of using an endoscope
- The success of tumor removal (resection rate)
It was found that endoscopy allowed for visualization and removal of tumor tissue that would otherwise have gone undetected in half of the cases in which it was used (38 out of 76 cases). The most common tumors removed via the eyebrow approach were meningiomas, gliomas, and metastatic tumors.
With regard to resection rates, 81.5% of the procedures in first-time patients resulted in total tumor removal, and 72% of the procedures in patients who had undergone prior surgery resulted in total or near-total tumor removal. Thus, the rate of tumor removal was high, and the rate of major post-operative complications were low.
The SO approach is associated with certain side effects that are temporary in the great majority of patients, such as weakness of the forehead muscles (frontal paresis) and a temporary loss of sensation in the forehead (forehead hypesthesia). A focus of the paper was describing a modified approach that the PNI surgical team uses which involves an alteration to the location of the initial incision of tissue below the scalp; this modification preserves more nerve fibers that go to the frontalis muscle of the forehead and thus shortens the time for recovery for forehead muscle movements.

Conclusions
With our focus on quality of life, and maximal safe tumor removal, our approach to all brain, skull base and pituitary tumors is to use the most direct and effective yet least invasive route possible. For tumors near the optic nerves and chiasm, under or in the frontal lobe and some along the temporal lobe, the eyebrow craniotomy is our go-to approach.
Depending on the exact location and what key structures are involved, the alternative keyhole approaches are the mini-pterional (from the side of the head thru a small incision above the ear and behind the hairline) or through the nose (endoscopic endonasal). With these 3 approaches, we can reach a majority of tumors in the front of the head and skull base.
Surprisingly, at many institutions, traditional larger craniotomies are still performed for most brain and skull base tumors and the endoscope is rarely or never used to augment visualization of the surgical field.
We hope our article and other educational efforts will make use of these less invasive and highly effective approaches more widely practiced.
Reference
- The Supraorbital Eyebrow Craniotomy for Intra- and Extra-Axial Brain Tumors: A Single-Center Series and Technique Modification
Shaheryar F Ansari, MD, Amy Eisenberg, NP, Amanda Rodriguez, RN, Garni Barkhoudarian, MD, Daniel F Kelly, MD
About the Author

Daniel F. Kelly
Daniel F. Kelly, MD, is the Director of the Pacific Brain Tumor and Pituitary Disorders Centers at Providence Saint John’s Health Center in Santa Monica, CA. Considered to be one of the top neurosurgeons in the U.S., Dr. Kelly is internationally recognized in the field of minimally invasive keyhole surgery for brain, pituitary and skull base tumors. He continues to focus his efforts on advancing innovative treatments for patients, providing fellowship training in minimally invasive neurosurgery, and patient education and support.
Last updated: February 23rd, 2021