

Study finds abdominal body fat linked to brain shrinkage, possible dementia
by Guest Author
An international study reveals a link between abdominal body fat and brain atrophy, potentially leading to dementia. Explore the groundbreaking findings from Pacific Neuroscience Institute’s Brain Health Center, shedding light on how abdominal fat affects brain health and Alzheimer’s risk. Learn how this research can influence early intervention and healthier lifestyles to mitigate dementia risks.
SANTA MONICA, Ca. (Aug. 29, 2023) – People with higher levels of abdominal body fat are at greater risk of having brain atrophy with aging, according to an international study that included a team of clinical researchers from Pacific Neuroscience Institute’s Brain Health Center, located at Providence Saint John’s Health Center.
Study participants with more of two types of abdominal body fat – subcutaneous fat under the skin and hidden visceral fat wrapped around the organs in the abdomen – are more likely to have loss of brain cells that might lead to dementia than people with smaller amounts of these types of abdominal fat, according to a study published today in the journal Aging and Disease.
The study used deep learning, a type of machine learning and artificial intelligence, to draw conclusions from whole body imaging scans. It also builds upon earlier research correlating fat and brain atrophy. The new study utilized much higher resolution imaging, included far more subjects, broadened the age range and expanded criteria to include subcutaneous fat. It also found women more than men are subject to brain shrinkage based on fat levels.
“Magnetic resonance imaging that encompassed the abdomen and head helped us determine both higher visceral and subcutaneous abdominal fat volume predicts loss of brain volume, a key metric of brain health,” said lead study author Cyrus A. Raji, MD, PhD, of Washington University in St. Louis, who collaborated with the research team at the Pacific Brain Health Center.
“By conducting MRI in a large sample of adults spanning a wide age range, our study identifies patterns of brain shrinkage and links those findings to important contributors such as abdominal fat,” said Somayeh Meysami, MD, assistant professor of neurosciences at Saint John’s Cancer Institute and a study co-author.
“When we identify those at higher risk of Alzheimer’s disease, evidence from research like this motivates healthier behaviors in early and mid-life when changes make the most difference in patient care outcomes,” said study co-author David Merrill, MD, PhD, director of the Brain Health Center.
For the study, 10,001 healthy people aged 18 to 90 years old had whole body scans with MR imaging machines. Deep learning was used to determine the volume of 96 brain regions. The same scan also was used to find the amount of visceral and subcutaneous abdominal fat on the scans. Then researchers looked to see if there was a link between these types of abdominal fat and brain volume.
After controlling for factors that could affect brain volume, such as age and the total volume inside the skull, researchers found higher amounts of both visceral and subcutaneous fat were associated with greater atrophy in the overall gray and white matter of their brains and the main lobes of the brain. Increased subcutaneous and visceral fat also was associated with cell loss in the hippocampus area of the brain and other areas associated with memory and thinking skills that are affected by dementia.
For people who were overweight and obese with high visceral fat, those aged 20 to 39 had nearly six times the risk for overall brain atrophy when compared to people of similar age with normal levels of visceral fat; those 40 to 80 had over five times the risk.
For the same groups of people who had high visceral fat, when looking at white matter atrophy in particular, people aged 20 to 39 had almost four times the risk when compared to people with normal visceral fat levels; those aged 40 to 59 had over four times the risk; and people aged 60 to 80 had over five times the risk.
The results from this large data set were contextualized down to individual examples when comparing two MRI scans in two participants from the study with the same age and sex:
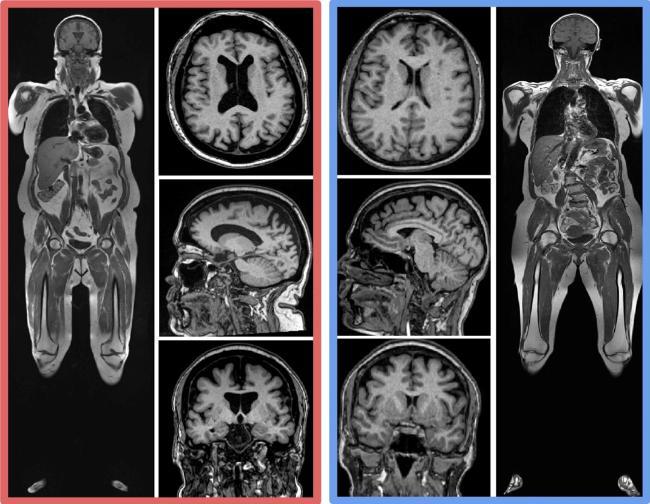
The study also found that women experienced a higher correlation between increased body fat and lower brain volume compared to men.
“Women are disproportionately affected by Alzheimer’s disease, and we have a growing understanding of biological sex-related risk factors. Prior research has shown obesity is a modifiable risk factor for dementia and prevention has become a cornerstone of dementia risk reduction management,” said Kellyann Niotis, M.D., a study co-author, preventive neurologist and Early Medical and brain health researcher at the Institute for Neurodegenerative Diseases-Parkinson’s & Alzheimer’s Research Education Foundation in Boca Raton, Fla.
Up to 40% of worldwide dementia cases are linked to 12 modifiable risk factors including obesity, according to a 2020 Lancet Commission report and the fact that women have a higher risk of Alzheimer’s disease. “We need additional research to better understand sex differences and brain health,” Dr. Merrill said.
A limitation of the study was that images were taken at one time and participants were not followed to see who developed dementia over time. Dr. Raji notes in future studies, researchers plan to follow participants over a period of time.
Such work opens the possibility of future treatment trials where both body fat and brain imaging can track the outcomes of such treatment efforts. Rajpaul Attariwala, M.D., Ph.D., study senior author noted, “The AI tools we have built to analyze this large whole body MRI data set have wide-ranging utility for the preventive health space, as well as for the pharmaceutical industry as they can be used to determine what the future implication of monitoring body fat and brain volumes will be. Currently, we do not know how interventions such as diet, exercise and weight loss drugs will affect the anatomical fat distributions in the body or if they may have secondary benefits for the brain.”
Adapted from a press release by Providence Southern California.
Media Coverage
Useful Links:
- Pacific Brain Health Center
- Brain Health Clinical Trials and Research
- Dementia
- Alzheimer’s Disease
- Mild Cognitive Impairment
- Memory loss
Related Videos
 Brain Health Dynamic Duo | Dr. Jennifer Bramen & Dr. Karen Miller
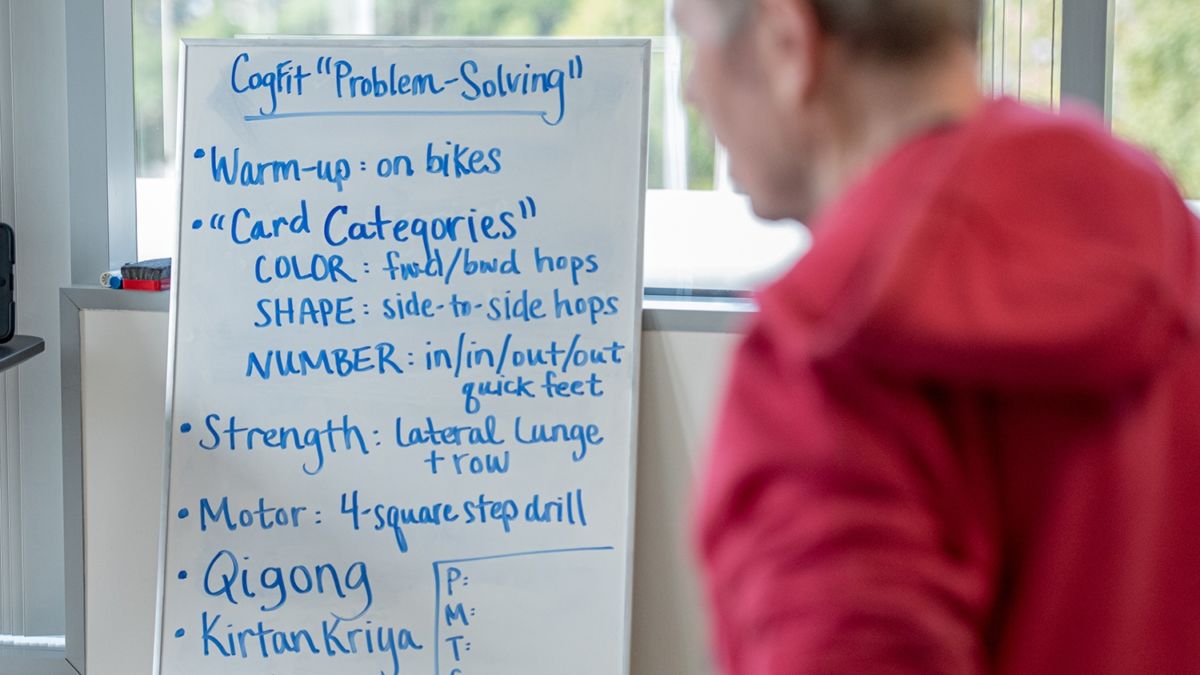
Strange though it may seem, we can tone our brain tissue the same way we tone our muscles. The fitness of our gray matter depends on how well we take…
Brain Health Dynamic Duo | Dr. Jennifer Bramen & Dr. Karen Miller
Strange though it may seem, we can tone our brain tissue the same way we tone our muscles. The fitness of our gray matter depends on how well we take…
 6 Ways to Improve Your Brain Health Through Lifestyle
Dr. Sarah McEwen, PhD, talks about ways to improve brain health through lifestyle choices.
6 Ways to Improve Your Brain Health Through Lifestyle
Dr. Sarah McEwen, PhD, talks about ways to improve brain health through lifestyle choices.
 Brain Health Center Research
Brain Health Center Research
 Brain Health Center Overview
Brain Health Center Overview
 12. It Takes A Village: Managing and Planning When the Diagnosis is Dementia, Sheila Moore, LCSW
12. It Takes A Village: Managing and Planning When the Diagnosis is Dementia, Sheila Moore, LCSW
 Beating the Odds on Alzheimer’s Disease | Molly Rapozo, MS, RDN, CD and Judy Davidson
Beating the Odds on Alzheimer’s Disease | Molly Rapozo, MS, RDN, CD and Judy Davidson
 Think Neuro Podcast: Alzheimer’s: Too Common and So Mysterious | Dr. Verna Porter
One in ten Americans who are 65 and older suffer from Alzheimer’s dementia. It’s the 6th leading cause of death in the country, and it is a scourge worldwide. But…
Think Neuro Podcast: Alzheimer’s: Too Common and So Mysterious | Dr. Verna Porter
One in ten Americans who are 65 and older suffer from Alzheimer’s dementia. It’s the 6th leading cause of death in the country, and it is a scourge worldwide. But…

Brain Health Dynamic Duo | Dr. Jennifer Bramen & Dr. Karen Miller

6 Ways to Improve Your Brain Health Through Lifestyle with Dr. Sarah McEwen, PhD
Brain Health Center Research

Brain Health Center Overview
12. It Takes A Village: Managing and Planning When the Diagnosis is Dementia, Sheila Moore, LCSW

Beating the Odds on Alzheimer’s Disease | Molly Rapozo, MS, RDN, CD and Judy Davidson

Alzheimer’s: Too Common and So Mysterious | Dr. Verna Porter
Related Articles
Last updated: July 11th, 2025



