Facial Reanimation Surgery
What is Facial Reanimation Surgery?
Facial reanimation surgery is a specialized surgical approach designed to restore facial movement and symmetry in individuals with facial paralysis. This paralysis can result from various causes, including facial nerve damage due to trauma, tumors, Bell’s palsy, or other neurological conditions. The goal of facial reanimation surgery is to improve both the functional and aesthetic aspects of facial expressions.
Several surgical techniques may be employed in facial reanimation surgery, depending on the underlying cause and extent of facial nerve damage
As the time from facial nerve injury increases, atrophy and scarring will occur in the facial muscles. Unlike the treatment options for acute facial nerve paralysis which are almost always aimed at reinnervating functional facial muscles, the treatment options for chronic facial nerve paralysis (greater than 1 year) can be separated into two broad categories of reversible and irreversible injuries.
In cases where it is unknown whether the patient has reversible or irreversible facial nerve injury, history, physical exam and diagnostic electrophysiologic testing are essential.
Patients with functional facial muscles have reversible injuries, and treatment is aimed at reinnervation of these muscles through repair of the facial nerve or transferring another nerve to power the branches of the the facial nerve close to the muscles of the face.
Patients whose facial muscles are no longer functional have irreversible injuries and typically require muscle transfers or static slings to restore facial form and function.
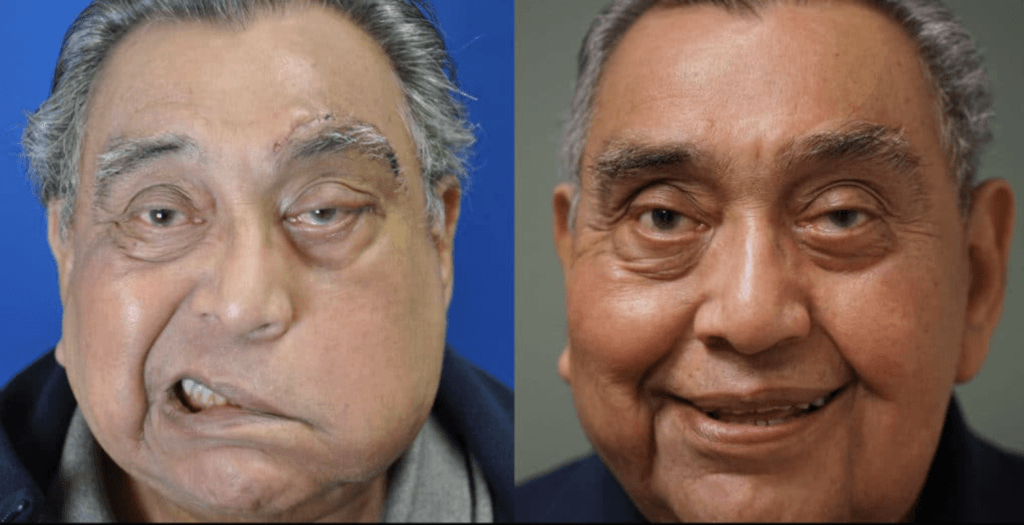
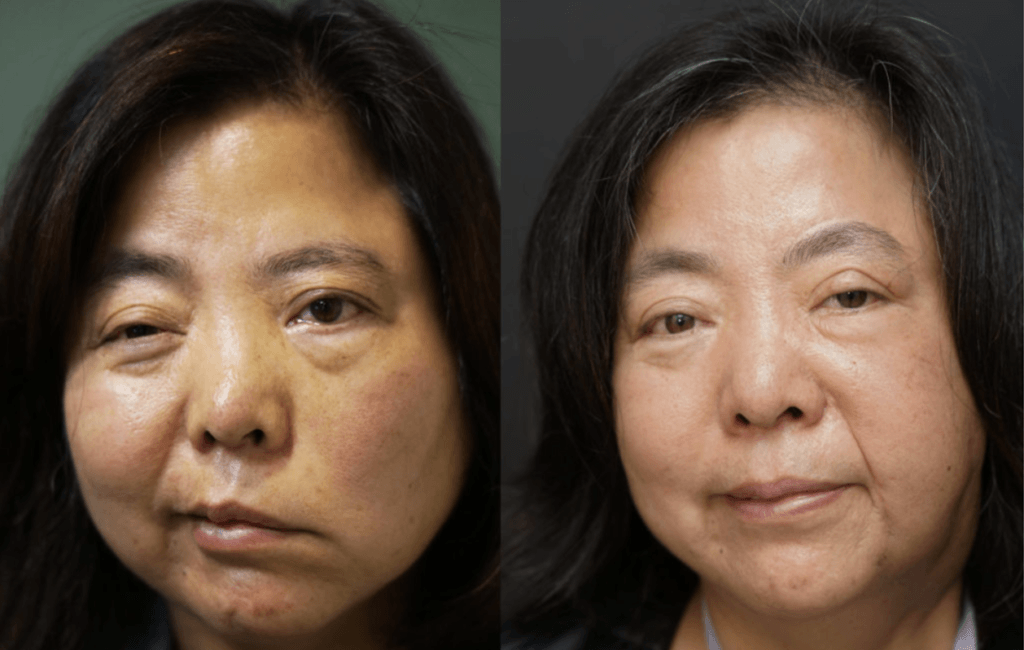
Photo Gallery | Before & After Facial Reanimation
Static Procedures
Static procedures do not lead to active purposeful movement. However, static facial reanimation plays an essential role in the treatment of facial paralysis and should not be overlooked. Static facial reanimation relies heavily on elevation and positioning of several key areas on the face and is often performed in combination with dynamic procedures, or those that do lead to purposeful movement.
Static suspension is often performed on the following areas:
- Elevating the droopy eyebrow to prevent visual field obstruction and to create symmetry with the opposite side
- Elevating the nasal ala and midface to improve breathing and repair collapse of the external nasal valve which is affected by facial paralysis
- Elevating the droopy oral commissure of the affected side to provide immediate restoration of symmetry. Elevation of the oral commissure not only provides symmetry but can also make it easier to speak, eat and drink on the affected side. This can be done in combination with nerve reinnervation or muscle transfer to correct asymmetry while waiting for the new nerves and muscles to activate.

Dynamic rehabilitation
Dynamic rehabilitation is required to restore facial tone, symmetry and purposeful synchronized facial movements.
Various options exist for dynamic facial nerve reanimation that includes:
- Nerve grafting
- Crossover techniques
- Nerve transfer or transposition
- Local muscle/tendon transfer
- Free muscle transfer

Nerve grafting for acute facial nerve injury
For reversible injuries, nerve grafting is a frequently used technique to repair “gaps” in the facial nerve. This requires taking a nerve from a different part of the body (i.e. sural sensory nerve) and then placing it between the 2 cut facial nerve ends to reinnervate the facial muscles.
Nerve grafting is most often performed after acute facial nerve injury (e.g. radical parotidectomy with nerve sacrifice, traumatic injury, or removal of an acoustic neuroma with known facial nerve transection). Nerve grafting is best performed at the time of injury or within the first 72 hours of nerve injury so that a nerve stimulator may be unable to identify the cut ends of the facial nerve. Therefore it is not a recommended option for the management of chronic facial paralysis.
Cross facial nerve grafting
For treatment of chronic facial paralysis, we use the cross facial nerve graft, nerve transfer/transposition and muscle transfer techniques.
The technique of cross facial nerve grafting with a donor nerve (e.g. sural nerve) is a useful technique when the main trunk of the facial nerve cannot be accessed or is beyond repair and the remaining peripheral branches in the face are spared. Cross facial nerve grafting alone is most effective in cases with denervation time of less than 6 months.
In patients with facial paralysis injury greater than 6 months, the cross facial nerve graft alone is not believed to be as effective and therefore is usually done in combination with a strong motor nerve transfer/transposition at the same time. Typically this involves using the nerve to masseter or the hypoglossal nerve as well.
Nerve transposition
For reversible facial nerve injury, nerve transfer/transposition involves using a different motor nerve to reinnervate the facial nerve and thus stimulate the facial muscles. Most commonly, the nerve to the masseter and hypoglossal nerve are used. The 5-7 and 12-7 transfer procedures do not create mimetic smiles that are synchronized to the opposite, normal face, however, with the addition of biofeedback and neuromuscular retraining, patients may achieve coordinated facial movements.
Loco-regional muscle and tendon transfer
When irreversible injury of the facial nerve occurs, the muscles of the face atrophy and are no longer able to function properly.
Therefore, transfer of new muscle may be required for dynamic facial reanimation. Historically, the temporalis muscle was transferred from the scalp down to the mouth to create dynamic movemebt of the lower face (i.e. smile). However, this would often lead to a defect in the side of the scalp, and excess bulk in the cheek that was non anatomic. Modification to this procedure have taught us that we do not need the entire temporalis muscle to create a smile, but can use the temporalis tendon.
Furthermore, this can be done in a minimally invasive fashion. Similar to the 5-7 nerve transfer, the temporalis tendon transfer allows for symmetry at rest, and formation of a smile when making a chewing motion on the affected side. While it does not lead to a synchronized, mimetic, smile, temoporalis tendon transfer can translate into a spontaneous controlled smile with intensive neuromuscular retraining and physical therapy.
Gracilis free flap (microneurovascular) procedure
The gracilis free flap is the gold standard procedure for dynamic facial reanimation to produce synchronous, mimetic facial movement in patients with irreversible chronic facial paralysis. It may be performed in 1 or 2 stages and requires a surgeon who is technically skilled in microsurgery. The procedure involves transferring a muscle from the thigh (gracilis) with its arterial and venous blood supply, and its nervous input to the face. The gracilis muscle is uniquely suited for this procedure due to its size, shape, length, reliable blood supply, and long single motor nerve (obturator nerve). There is minimal morbidity to the thigh and the scar is easily hidden as well.
The traditional gracilis free flap for facial reanimation involved a first stage cross-face nerve graft followed by the free flap 6-12 months later. However, single stage gracilis free flaps powered by the nerve to masseter also provide excellent and predictable results, however, mimetic smile is less likely as one must bite or chew to initiate smile. A third option is to perform dual innervation of the gracilis muscle using both the cross face nerve graft and the nerve to masseter.
Management of the eye
For all patients with facial paralysis, appropriate early eye care is essential to prevent corneal injury and infection that can lead to blindness. All patients should use artificial tears, eye lubrication, moisture chambers, and protective eye taping.
Patients with the following symptoms are at higher risk for injury to the eye:
- In ability to close your eye completely
- Reduced corneal sensation
- History or presence of dry eye
- More pronounced, larger eyes
Upper eyelid weight placement
Upper eyelid weights (platinum typically) may be surgically placed under the eyelid skin to assist with eyelid closure. For patients with the possibility of facial nerve recovery, surgically placed eyelid weights may be removed if function returns or can stay indefinitely.
Lower eyelid repositioning
If the lower eyelid becomes too relaxed after facial paralysis, it may pull away from the eye. This is called paralytic ectropion and can lead to incomplete closure, excessive tearing and increase the risk of injury. Shortening of the lower eyelid can be performed under local or general anesthesia. This procedure is routinely performed with upper eyelid weight placement to improve eyelid closure and protect the eye from exposure related injury.
Patient support for facial paralysis
We offer real-time psycho-social support with an on-site social worker. There are a number of resources available to patients.
Dr. Amit Kochhar hosts an educational facial nerve webinar series.
Websites of interest
- Acoustic Neuroma Association
- Subscriber-only site for patients diagnosed with Acoustic Neuroma
- Request to view Dr. Kochhar’s lecture on synkinesis
- Facial Palsy UK
- An excellent resource to learn about conditions associated with facial paralysis and treatment options.
- Ascend PT (Orange County, California)
- Physical Therapists with specialty training in facial paralysis
Useful links
- Bell’s Palsy and Facial Paralysis Support Group
- Dr. Kochhar’s lecture on Synkinesis
- Dr. Kochhar’s lecture on Bell’s Palsy and Synkinesis Frequently Asked Questions
- Bell’s Palsy and Synkinesis-Long Timers
- Dr. Kochhar and Dr. Barkhadourian’s lecture on Facial Paralysis and Facial Pain
- Acoustic Neuroma Association
- Dr. Kochhar’s hosted lectures

In-Person or Virtual Video Visit
Our specialists have consultation openings for new patients.