
Alzheimer’s Disease
What is Alzheimer’s disease?
Alzheimer’s disease is a progressive neurological disorder that affects the brain’s function and causes a gradual decline in cognitive function, including memory, thinking, and behavior. It is the most common cause of dementia, accounting for approximately 70% of all cases of dementia.
The exact cause of Alzheimer’s disease is not fully understood, but it is believed to be a combination of genetic, environmental, and lifestyle factors. The disease is characterized by the accumulation of abnormal proteins in the brain, which interfere with the communication between brain cells and cause their death over time.
There is no cure for Alzheimer’s disease, but there are medications available that can help manage the symptoms and slow the progression of the disease. These medications work by increasing the levels of neurotransmitters in the brain, which can improve communication between brain cells and delay the onset of more severe symptoms.
Lifestyle changes, such as regular exercise, a healthy diet, and cognitive stimulation, may also be helpful in managing the symptoms of Alzheimer’s disease. Additionally, it is essential to work closely with a healthcare professional experienced in treating Alzheimer’s disease to develop an appropriate treatment plan.
While Alzheimer’s disease is a devastating condition that affects millions of people worldwide, early detection and treatment can help individuals maintain their quality of life for as long as possible.
Differences Between Alzheimer’s Disease and Dementia
People often wonder about the difference between Alzheimer’s and dementia. Dementia is an “umbrella term” and not a specific disease. Dementia is a descriptive term for symptoms of mental and cognitive decline that are severe enough to interfere with an individual’s ability to perform everyday functions and activities.
Worldwide, 50 million people have Alzheimer’s and other dementias. Vascular dementia, which occurs after a stroke or with vascular disease in the brain, is the second most common type of dementia.
However, there are many other conditions that can cause dementia symptoms, including some that are reversible, such as thyroid issues or various vitamin deficiencies. Alzheimer’s disease causes problems with memory, thinking and behavior and is often referred to as Alzheimer’s dementia.
Comprehensive Guide for Dementia Caregivers
Symptoms
The symptoms of Alzheimer’s disease can vary depending on the stage of the disease, but they typically include memory loss, difficulty with language and communication, impaired judgment, and changes in mood and behavior. As the disease progresses, individuals may experience more severe symptoms, such as difficulty with mobility, loss of ability to perform activities of daily living, and eventually, the loss of ability to recognize loved ones.
Early signs of Alzheimer’s include:
- Memory loss or impairment, such as difficulty remembering names, dates, events, appointments and details of conversations.
- Difficulty concentrating, planning or developing an appropriate solution to a problem.
- Problems with completing tasks in a timely and efficient manner at home or at work.
- Confusion or disorientation with details of place, situation or the passage of time.
- Visuo-spatial difficulties, such as geographical disorientation with driving, problems judging specific distances, or losing/misplacing items around the home.
- Language difficulties, such as word-finding problems, constricted/limited vocabulary or changes in the fluency of speech or writing.
- Demonstrating compromised reasoning or judgment in decision-making.
- Withdrawal from work or social activity, increased apathy and decreased interest in social engagements or events.
- Changes in mood, personality or behavior including signs of depression and anxiety.
Alzheimer’s disease typically progresses slowly. There are three basic Alzheimer’s stages classified as:
- mild (early stage)
- moderate (middle stage)
- severe (late stage)
Each patient’s progression through Alzheimer’s is unique, and the disease can present in a variety of ways in different individuals. Because of the progressive and neurodegenerative nature, each person will experience the advancement of signs and symptoms of Alzheimer’s dementia, but the specific timing and presentation of these will vary among different individuals.
Diagnosis
The diagnosis of Alzheimer’s disease, or other related dementias, depends on careful medical, cognitive and physical assessments, performed by our trained specialists to evaluate patients for cognitive changes and dementia.
The initial assessment may be performed by one or more of our following specialists:
- A geriatrician (trained to treat older adults)
- A neurologist (trained to treat brain/neurocognitive disorders)
- A geriatric psychiatrist (trained in mental/cognitive disorders of older adults)
We carefully review the patient’s medical and physical history, medication history and the presenting cognitive/behavioral symptoms, and follow-up tests are administered based upon these findings.
Alzheimer’s testing and evaluation
During the patient’s visit, an Alzheimer’s evaluation includes the assessment of:
- Whether there are impaired cognitive/memory or thinking skills compared to others in the same age group.
- Whether there are changes in mood, personality or behavior.
- The extent of cognitive, memory or thinking impairments or changes.
- How cognitive/thinking difficulties affect everyday life and function.
- Further testing and assessments with focus on determining the underlying cause of symptoms.
We may order additional laboratory tests, including brain scans or more detailed memory assessments such as formal neurocognitive or neuropsychological testing. Results can provide useful information for diagnosis, including ruling out other conditions that may cause similar symptoms like thyroid dysfunction and vitamin deficiencies.
Ruling out other conditions
We perform thorough analysis through blood work, imaging studies, and formal neurocognitive testing by a licensed neuropsychologist.
In addition, a physical examination is conducted to check for other health conditions that could be causing or contributing to symptoms, such as signs of past strokes, Parkinson’s disease, depression, or other medical conditions.
Diagnosing healthy aging versus Alzheimer’s disease
Through our memory evaluation process, we can confidently identify whether a patient’s brain is experiencing normal changes associated with healthy aging versus neurodegenerative disease such as Alzheimer’s disease, cerebrovascular disease, or other more rare causes of dementia such as Parkinson’s disease, Lewy body dementia or Frontotemporal dementia.
We complete a comprehensive history and information assessment, including getting inputs from patient, family, friends, caregivers, and previous healthcare providers.
Tests of neuropsychological function:
- Quantitative EEG brain mapping
- Evoked response potential (ERP) testing
- Brain imaging (volumetric magnetic resonance imaging)
When indicated, we include more involved biomarker testing such as cerebrospinal fluid sampling via lumbar puncture and/or positron emission tomography (PET) using specific radio-biomarkers such as glucose, amyloid, or dopamine.
Additional Alzheimer’s Testing
Additional diagnostic testing for Alzheimer’s disease may include:
- Mental status tests: To evaluate memory, thinking and problems-solving skills
- Brain mapping: To assess overall cognitive deficits associated with dementia
- Mood assessment: We evaluate the sense of emotional well-being to detect any signs of depression, anxiety or other mood disorders that can contribute to memory/cognitive problems, loss of interest in life, and other symptoms that can worsen cognition and even mimic the clinical presentation of dementia.
- Genetic testing: Researchers have identified certain genes that increase the risk of developing Alzheimer’s disease and other rarer “determinant” genes that directly cause Alzheimer’s. Although genetic tests are available for some of these genes, health professionals do not currently recommend routine genetic testing for all cases of Alzheimer’s disease.
- Brain imaging: A standard medical workup for Alzheimer’s disease or other dementias often includes structural imaging to rule out other conditions that may cause similar symptoms to Alzheimer’s disease. Researchers are studying other brain imaging techniques (e.g. amyloid and tau imaging) as a possible technique for enhanced diagnosis and tracking of the progress of Alzheimer’s disease.
- Blood and cerebrospinal fluid (CSF) biomarker tests
- Hormone testing, balancing and adjustment
- TMS
- Cognitive Remediation /Neurofeedback
Treatment
Conventional therapies for Alzheimer’s disease
One class of drugs used for symptomatic treatment of Alzheimer’s disease includes acetylcholinesterase inhibitors, which decrease the breakdown of the neurochemical, acetylcholine, which is important for proper nerve signaling in memory and learning. These drugs are symptomatic, which means that they may slow down the rate of progression of the disease, but they do not correct or reverse the disease. Common side effects are usually mild for these medications and may include diarrhea, vomiting, nausea, fatigue, insomnia, loss of appetite, and weight loss.
There are three main drugs in this class: donepezil (Aricept), galantamine (Razadyne), and rivastigmine (Exelon).
Aricept (donepezil) is the only treatment approved by the FDA for all stages of Alzheimer’s disease: mild, moderate, and severe. Aricept (donepezil) may be taken as a tablet that is swallowed, or as a wafer that dissolves in the mouth.
Razadyne (galantamine), formerly called Reminyl, is FDA approved for mild to moderate Alzheimer’s. This can be taken as a regular release tablet that works right away, an extended release capsule that gives off the medicine slowly, or in liquid forms. The FDA and other international health authorities are reviewing the safety of Razadyne (galantamine) after data from two clinical studies indicated that people taking the drug had a higher death rate than those taking a placebo (sugar pill). Based on this information, FDA has asked the manufacturer to revise the labeling.
Exelon (rivastigmine) is for people who have mild to moderate Alzheimer’s. The patch can be worn as a topical (skin) patch that releases the drug across the skin (trans dermally) or may be taken in capsule or liquid form.
In addition, Namenda (memantine) is FDA approved for moderate-to-severe Alzheimer’s disease. This medication reduces the actions of a chemical in the brain (i.e. glutamate) that may contribute to the symptoms of Alzheimer’s disease. This medicine works by changing the amount of a brain chemical called glutamate, which plays a role in learning and memory.
Namenda (memantine) has been associated with a moderate decrease in clinical deterioration, and only a small positive effect on cognition, mood, behavior, and the ability to perform daily activities in moderate to severe Alzheimer’s disease. This drug does not appear to be of benefit in the situation of mild disease. The drug may work best when taken with Aricept (donepezil), Exelon (rivastigmine), or Razadyne (galantamine). Namenda’s side effects include tiredness, dizziness, confusion, constipation, and headache.
Namzaric (memantine hydrochloride extended-release and donepezil hydrochloride) is a mix of two drugs. It is suggested for people with moderate to severe Alzheimer’s who are already taking the two drugs separately. This formulation has the convenience of a single pill with once-a-day dosing.
Doctors may also prescribe other medicines for additional medical concerns that coexist with Alzheimer’s dementia, such as depression, anxiety, sleep disturbances and behavioral problems like agitation and aggression.
Non-pharmacologic Interventions
The Bredesen Protocol
The Bredesen Protocol aims at treating and reversing symptoms associated with Alzheimer’s disease. It particularly hopes to improve cognition and reverse the cognitive decline associated with early Alzheimer’s disease as well as mild cognitive decline (MCI) and severe cognitive impairment (SCI).
The protocol uses lifestyle and nutritional recommendations in a 36-point system to treat many of the underlying contributors of disease. In an individualized approach and referring to aspects of this protocol, patients can receive a plan to help adjust biochemical and metabolic imbalances, working with diet including supplements, sleep, exercise and other lifestyle components.
Lifestyle
Adjusting lifestyle factors can help maintain and improve brain health. A few recommendations are listed below.
- Exercise: Studies show that aerobic exercise for 30 minutes three to four days a week improves memory, brain function and physical fitness.
- Healthy dietary practices: A Mediterranean or MIND diet rich in fruits, vegetables, olive oil, legumes, whole grains and fish offers many heart-healthy and brain-healthy benefits.
- Heart healthy behaviors: Control of blood pressure, cholesterol, blood sugars and smoking cessation can offer additional benefits for brain health and cognitive vitality.
- Avoiding head injury: Wearing a seat belt, bicycle helmet and avoiding falls that result in head injury is recommended.
- Enhancing mental activities: Reading, writing, learning a new language and other novel activities that stimulate the mind help to enhance cognitive agility improve functioning.
- Socializing: People who engage in regular social events and practices have better and more sustained cognitive functioning with age than those individuals who are more socially isolated.
- Sleep: Research is showing that sleep is an important and often neglected aspect of health. Seven to eight hours of sleep each night is thought to help minimize brain amyloid build up associated with Alzheimer’s dementia.
Clinical trials for Alzheimer’s disease
Eligible patients can participate in a clinical trial for Alzheimer’s disease where they will have access to the leading-edge diagnostics and treatment options such as stem cell therapy. If you are interested in any of our current studies on Alzheimer’s disease or if you are interested in participating in a research study but don’t currently see one that suits you, you can join our research registry to be placed on a list for future studies.
Early Onset Alzheimer’s Disease
Most commonly, Alzheimer’s disease and associated dementia impacts people over the age of 65. However a small percentage of instances, younger people can be affected by the disease when it is called early onset Alzheimer’s disease or younger onset Alzheimer’s disease. Alzheimer’s disease symptoms may begin in their 30s and 40s with the patient reaching the advanced stages of dementia in their 40s and 50s.
While all contributing factors to Alzheimer’s disease causes are not known, it is thought that, particularly in early onset Alzheimer’s, there is a genetic component.
Prevention of Alzheimer’s Disease
As this disease becomes more prevalent with aging of the world’s population, many specialists are focused on how to prevent Alzheimer’s disease or at least how to delay its onset. Amyloid and tau proteins that form abnormal brain deposits are linked to Alzheimer’s disease but other factors such as brain inflammation and vascular conditions may also involved.
Lifestyle plays an important role and adoption of some healthy strategies may help in Alzheimer’s disease prevention or delay. These include:
- Exercise: Studies show that aerobic exercise for 30 minutes three to four days a week improves memory, brain function and physical fitness.
- Healthy dietary practices: A Mediterranean or MIND diet rich in fruits, vegetables, olive oil, legumes, whole grains and fish offers many heart-healthy and brain-healthy benefits.
- Heart healthy behaviors: Control of blood pressure, cholesterol, blood sugars and smoking cessation can offer additional benefits for brain health and cognitive vitality.
- Avoiding head injury: Wearing a seat belt, bicycle helmet and avoiding falls that result in head injury is recommended.
- Enhancing mental activities: Reading, writing, learning a new language and other novel activities that stimulate the mind help to enhance cognitive agility improve functioning.
- Socializing: People who engage in regular social events and practices have better and more sustained cognitive functioning with age than those individuals who are more socially isolated.
- Sleep: Research is showing that sleep is an important and often neglected aspect of health. Seven to eight hours of sleep each night is thought to help minimize brain amyloid build up associated with Alzheimer’s dementia.
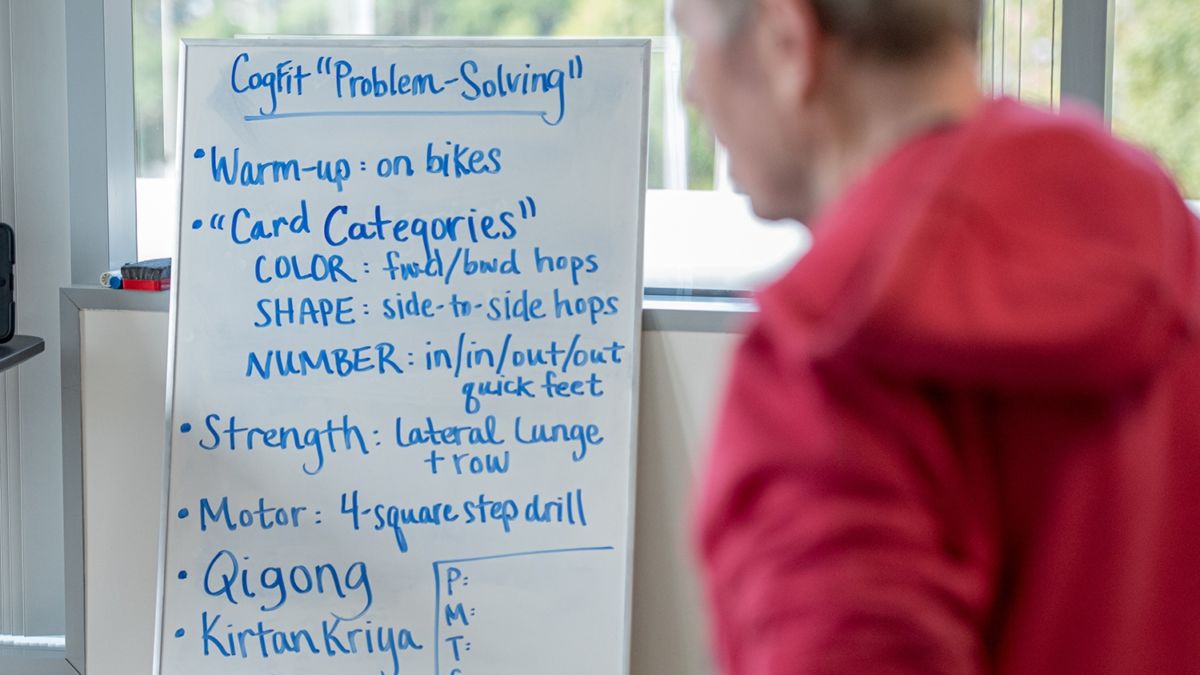
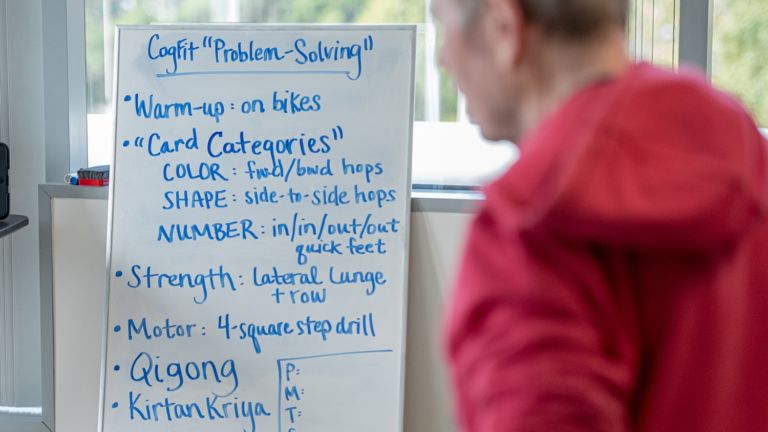
Alzheimer’s Disease Patient & Caregiver Support
For patients and families affected by this progressive and debilitating disease, coping with Alzheimer’s dementia can be challenging and frustrating. The Pacific Brain Health Center provides support for patients and their families with extensive exercise classes and support groups. We offer balance classes and mindfulness/yoga classes along with support groups for patients with dementia co-facilitated by medical and spiritual faculty and guest speakers.
There are many other community resources for family caregiver support and to help navigate through the struggles of living with Alzheimer’s disease.
Alzheimer’s and Related Dementias Caregiver Support Group
- Alzheimer’s Association
- Wise and Healthy Aging
- Alzheimer’s Los Angeles
- Opica
Support for older adults with memory loss and their families
11759 Missouri Ave. Los Angeles, CA 90025 T: 310.478.0226 - MPTF (entertainment industry)
- Asian Pacific Islander Dementia Care Network
- Alzheimers.net
Videos Related to Alzheimer's Disease
 Alzheimer’s LA Caregiver Tips
Alzheimer’s LA Caregiver Tips
 Brain Health Center Overview
Brain Health Center Overview
 Brain Health Center Research
Brain Health Center Research
 Meet Dr. Merrill
David A. Merrill, MD, PhD, is an adult and geriatric psychiatrist with double-board certification by the American Board of Psychiatry and Neurology. He is director of the Pacific Brain Health…
Meet Dr. Merrill
David A. Merrill, MD, PhD, is an adult and geriatric psychiatrist with double-board certification by the American Board of Psychiatry and Neurology. He is director of the Pacific Brain Health…
 Meet Dr. Porter
Dr. Porter is the Director of Dementia, Alzheimer’s disease, and Neurocognitive Disorders at the Pacific Brain Health Center at Pacific Neuroscience Institute (PNI) located at Providence Saint John’s Health Center…
Meet Dr. Porter
Dr. Porter is the Director of Dementia, Alzheimer’s disease, and Neurocognitive Disorders at the Pacific Brain Health Center at Pacific Neuroscience Institute (PNI) located at Providence Saint John’s Health Center…
 Meet Dr. Scott Kaiser
Dr. Scott Kaiser, a board-certified family physician and geriatrician, is the Director of Geriatric Cognitive Health and provides specialty geriatric medical consultations at the Pacific Brain Health Center. Focused on…
Meet Dr. Scott Kaiser
Dr. Scott Kaiser, a board-certified family physician and geriatrician, is the Director of Geriatric Cognitive Health and provides specialty geriatric medical consultations at the Pacific Brain Health Center. Focused on…
 Think Neuro Podcast: Alzheimer’s: Too Common and So Mysterious | Dr. Verna Porter
One in ten Americans who are 65 and older suffer from Alzheimer’s dementia. It’s the 6th leading cause of death in the country, and it is a scourge worldwide. But…
Think Neuro Podcast: Alzheimer’s: Too Common and So Mysterious | Dr. Verna Porter
One in ten Americans who are 65 and older suffer from Alzheimer’s dementia. It’s the 6th leading cause of death in the country, and it is a scourge worldwide. But…

Alzheimer’s LA Caregiver Tips

Brain Health Center Overview
Brain Health Center Research

Meet Dr. Merrill
Meet Dr. Porter

Meet Dr. Kaiser

