Vagus Nerve Stimulation (VNS)
Vagus Nerve Stimulation for Epilepsy and Depression
Vagus nerve stimulation (VNS) is a treatment option that is currently approved in the US and limited to the treatment of intractable epilepsy and treatment-resistant depression.
What is Vagus Nerve Stimulation (VNS)?
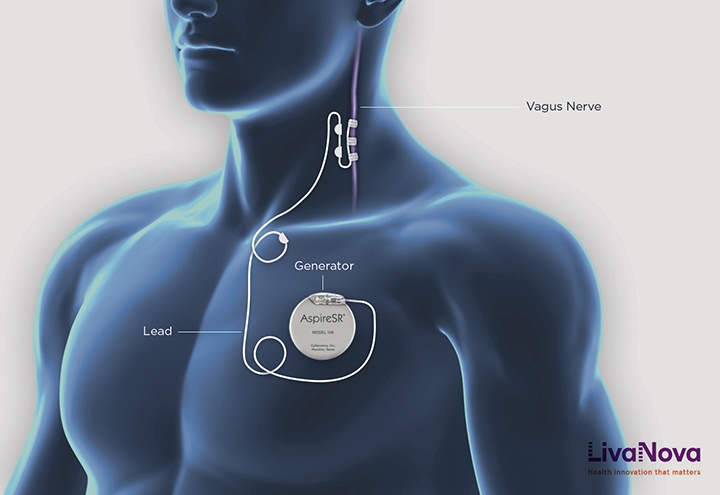
Vagus nerve stimulation (VNS) utilizes a device to deliver electrical impulses to the vagus nerve, which is present on both sides of the body. This large nerve originates from the brainstem and travels through the neck area to terminate in several organs including the heart, the lungs and the gastrointestinal system. It participates in several critical functions including heart rate control, peristalsis and regulating the size of airways opening. When stimulated, electrical impulses are sent to various regions of the brain, resulting in altered brain activity to manage specific conditions. Stimulating the vagus nerve appears to stabilize abnormal electrical activity by sending regular, mild pulses of electrical energy to the brain through the vagus nerve.
There are multiple methods and devices available for VNS. Notably, an implantable vagus nerve stimulator or pulse-generator device similar to a pacemaker has been approved by the Food and Drug Administration (FDA) for the treatment of epilepsy and depression. This device functions by sending electrical stimulation to brain areas involved in seizures and mood regulation thereby controlling seizures due to epilepsy and managing symptoms of treatment-resistant depression.
- In patients with epilepsy, VNS regulates electrical signals to the brain, which can help reduce seizure frequency and intensity.
- In patients with treatment-resistant depression, VNS activates the brain’s mood centers, potentially alleviating symptoms of depression.
Patients undergoing VNS often experience improvements in their emotional state and neurological health, making it a valuable tool for those who have not responded well to traditional nerve or nervous system treatments.
While the effect of VNS is on the brain, the procedure does not include brain surgery. Once the pulse generator is programmed after surgery, patients do not generally feel the pulses. The device is surgically implanted beneath the skin of the chest, with a wire threaded under the skin to connect it to the left vagus nerve. Upon activation, the device transmits electrical signals along the left vagus nerve to the brainstem, subsequently influencing brain function. The right vagus nerve is typically not used due to a higher likelihood of affecting cardiac function.
Indications
Epilepsy and depression are debilitating conditions caused by irregular brain activity affecting the entire lifespan of a patient as well as their caregivers. Fortunately, neuromodulation with the use of VNS may offer hope for those suffering from these conditions.
VNS for Epilepsy
Patients suffering from epilepsy can be considered for VNS if they have failed a proper trial of at least two (2) anti-epileptic medications. VNS does not replace medications and the therapy is added on the regime that works the best for the patient. Although not curative, VNS can improve seizure control in those patients and the therapeutic effect tends to increase over time. On average, patients experience approximately a 25% reduction in seizure frequency after three months of therapy, and the benefits increase over time. Approximately 50%-60% of patients will experience a 50% reduction in seizure frequency after two years of therapy. This improvement in efficacy over time is likely the result of progressive device programming and broad neuromodulatory changes in the epilepsy network. Despite being used in the clinical setting for several years, the mechanism of action of VNS is not fully understood. It is thought that the stimulation leads to modulation in the local brainstem circuitry; in turn, these local circuits engage more widespread pathways leading to desynchronization in the epileptogenic zones.
The broad effects of VNS make this therapy beneficial for patients with multifocal or generalized epilepsy where a specific seizure focus cannot be identified and treated surgically. As VNS does not require the identification of a focus, it still results in reduced seizure frequency.
Vagus Nerve Stimulator for Depression
Initial clinical experience suggested that VNS may improve depression. Epilepsy patients undergoing stimulation therapy treatment with VNS reported enhanced mood, even in cases where the seizure frequency was not reduced. Subsequent dedicated clinical trials demonstrated that VNS can reduce the severity of major depression by about 30%. Patients with depression of moderate severity and who have experienced some improvement with medication are more likely to benefit from VNS therapy.
VNS is not curative for depression but it can add another dimension to the overall treatment plan. Patients who undergo this therapy should continue to closely follow the recommendations of their mental health providers. In particular, patients should continue to take their medications and attend their therapy sessions.
Patients with a VNS implant for depression often see gradual improvements, which may continue to develop over several months of stimulation therapy. Benefits reported include:
- Reduction in depression symptoms
- Improved mood and quality of life
- Enhanced response to conventional antidepressants
While VNS is safe for many, it can cause side effects such as hoarseness, throat pain, or changes in voice tone due to stimulation of the nerve. There is also the general risk associated with surgical procedures, including infection or complications from anesthesia.
VNS Surgical Procedure
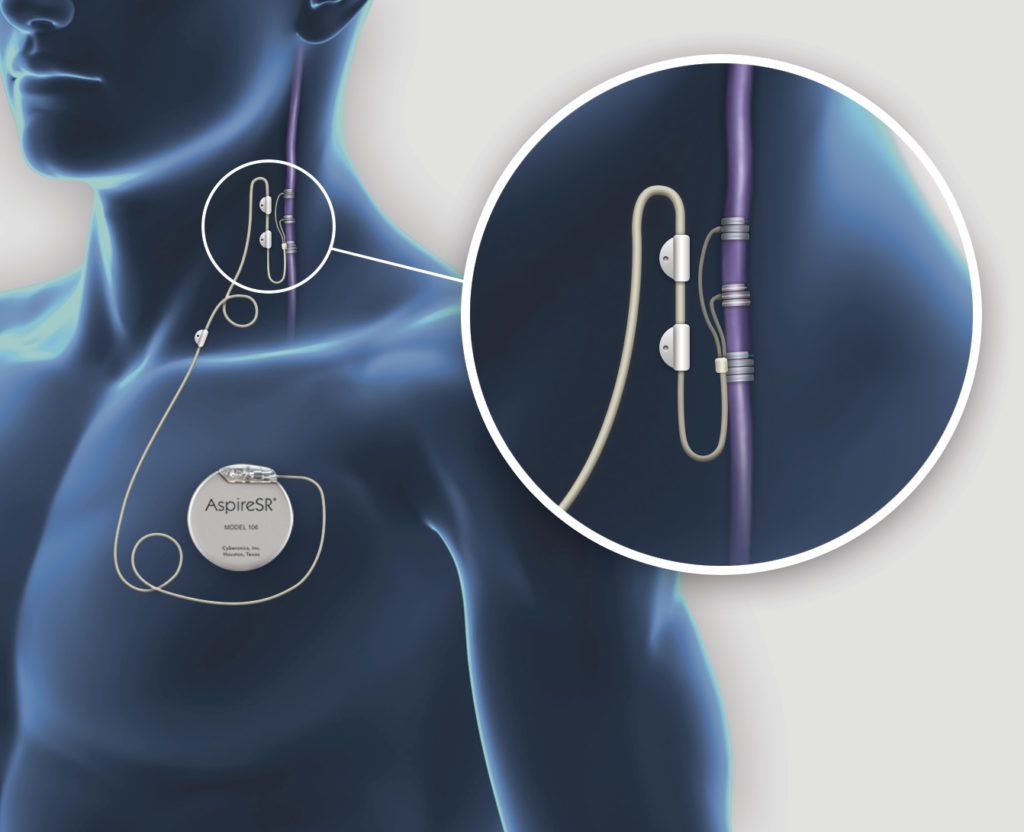
VNS surgery involves the insertion of two main components: the lead and the generator. The lead is inserted through a small incision in the anterior mid-neck area. Through this incision, the vagus nerve is identified and isolated and the dedicated lead is gently secured to it. The preferred method is to implant the device on the left side of the body.
The generator is inserted in the upper chest area. Through technological advancements, the size of the pulse generator has reduced over time. Therefore, the insertion requires only a small incision typically located about 1 inch under the clavicle. It is secured in place to the subcutaneous tissue. Finally, the lead is tunneled under the skin from the neck to the chest; all of the components are discretely implanted under the skin.

There are a few options available for the implanted generator. For example, one generator senses the heart beat and can trigger an additional electrical pulse when the heart rate exceeds a predetermined level. This type of system can be beneficial for patients who tend to experience a higher heart rhythm at the onset of a seizure. Another generator is designed to hold a longer battery life which can be advantageous for patients requiring stronger electrical stimulation. Finally, another model possesses a discreet profile.
VNS Post-operative Care
After VNS surgery, patients generally remain in the hospital for one day. We recommend keeping the wounds dry for a few days and to avoid irritating the surgical sites to help prevent infection.
The patient should plan to meet with their neurologist, in the case of epilepsy, or their psychiatrist, in the case of depression within a month of the surgery.
VNS Device Programming
The electrical impulse produced by the vagus nerve stimulator is adjusted by the physician’s programmer. The programmer communicates non-invasively with the implanted device. Typically, the generator is adjusted gradually over time to make sure that the stimulation is well-tolerated. Possible side-effects from vagal nerve stimulation include hoarseness of the voice and shortness of breath.
VNS is administered in cycles. The pulse is sent for a few seconds every few minutes. The providers can adjust the intensity and the frequency of the pulse as well as the duration of the on/off cycles. The patient may elect to administer additional impulses using a magnet provided with the device. This feature is especially useful in patients who can feel an aura or sensation before a seizure.
VNS Specialists
Clinic Location
1301 20th St, #150, Santa Monica, CA 90404
310-582-7641
FAQs about Vagus Nerve Stimulation
What are the symptoms of an overstimulated vagus nerve?
Vagus nerve stimulation (VNS) is a treatment primarily used for epilepsy aimed at reducing the frequency and intensity of seizures. However, when the vagus nerve is overstimulated, it can lead to specific symptoms that patients need to be aware of.
Common signs of an overstimulated vagus nerve include:
- Sudden changes in heart rate: Patients might experience either a significant increase or decrease, which can feel alarming.
- Gastrointestinal issues: These may range from abdominal pain and nausea to changes in bowel movements.
- Altered breathing patterns: This could manifest as shortness of breath or a feeling of tightness in the chest.
Additionally, patients may report feeling lightheaded or having an unusual tingling sensation in the neck or throat area. If you experience any of these symptoms, contact your healthcare provider immediately. Managing the intensity of VNS can help mitigate these effects and maintain the benefits of the treatment for controlling seizures.
What happens when the vagus nerve is under-stimulated?
When the vagus nerve is under-stimulated, it can lead to a decrease in its regulatory functions, affecting both physical and mental health. Vagus nerve stimulation (VNS) is often used to manage epilepsy and prevent seizures, so insufficient stimulation might result in an increased frequency or severity of seizures.
Additionally, the vagus nerve plays a crucial role in regulating heart rate and digestion. An under-stimulated nerve may cause:
- Digestive issues: Patients might experience slowed digestion, constipation, or abdominal discomfort.
- Heart irregularities: There could be an inconsistency in heart rate, potentially leading to palpitations or feelings of anxiety.
Mental health can also be impacted, as the vagus nerve influences mood and stress levels. Lack of adequate stimulation might lead to heightened stress responses or difficulty managing anxiety.
Ensuring proper stimulation of the vagus nerve is important for VNS therapy. Discussing symptoms with a specialist at Pacific Neuroscience Institute® can help tailor VNS treatments to maintain optimal brain stimulation and overall well-being.
What organs does the vagus nerve affect?
The vagus nerve impacts a broad range of organs. The primary function of the vagus nerve is afferent, conveying information from internal organs such as the gut, liver, heart, and lungs to the brain. This indicates that the internal organs are significant sources of sensory information for the brain. The vagal nerve is essential for maintaining homeostasis.
Key organs influenced by the vagus nerve include:
- Heart: It helps control heart rate and blood pressure, making its function crucial for cardiovascular health.
- Lungs: The nerve aids in managing breathing patterns.
- Digestive tract: It stimulates muscle movements that propel food through the GI tract and regulates the release of digestive enzymes.
Vagus nerve stimulation (VNS) is a technique used not only to treat epilepsy by reducing seizure frequency but also to positively impact depression and anxiety through its neural pathways. Ensuring that this nerve functions correctly is important for the effective regulation of these bodily systems. VNS therapy supports broad aspects of physical health and emotional well-being.