Craniopharyngioma: Brain Tumor Causing Visual Loss
” The staff of doctors, their assistants, the nurses and the rest of the staff went above and beyond the call of duty to help make my stay very comfortable. “
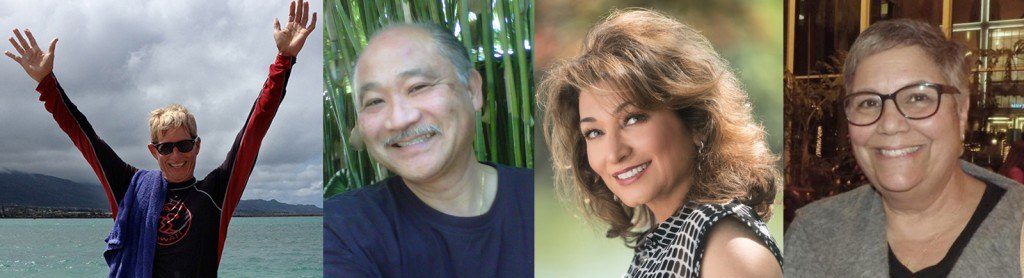
– Odette P. Supraorbital Eyebrow Approach
My Journey to Recovery

When Odette P., 47, from Denver, CO, found out she had a benign brain tumor called a craniopharyngioma in November of 2008, she didn’t hesitate to fly the over 800 miles to Southern California to meet with Daniel Kelly, MD, Director of the Brain Tumor Center at the Saint John’s Cancer Institute at Saint John’s Health Center, to see what could be done.
Odette first started having headaches and blurred vision in September of 2008. She blamed her vision problems on the LASIK eye surgery she had earlier that year and thought the headaches were due to allergies. She went to her general practitioner with her concerns and was told to up her water intake and take Claritin—an over-the-counter allergy relief medication.
By November 2008, Odette’s symptoms hadn’t diminished, so she took it upon herself to see an optometrist. “He discovered during my exam that I had no temporal vision,” Odette said. “He advised that I urgently contact my GP and tell her I needed to have an MRI.”
Understanding the Options
Odette scheduled an MRI for the next day and within a few days had the results.“When I found out about the tumor, I contacted my sister, who is a radiation therapist at the VA Hospital in Los Angeles. A friend of hers is a personal friend of Dr. Kelly,” Odette said. “She found him for me. Thank God!” Odette and her husband talked to Dr. Kelly and his assistant Maribel Leyva about her options. “They couldn’t have been more thorough in explaining the good and bad of my situation and what needed to be done,” Odette said. After the conversation, Odette decided to fly from her home in Denver to Santa Monica and meet with Dr. Kelly in person and look into what treatment options were available to her.
“Craniopharyngiomas are relatively uncommon benign tumors that arise near the pituitary gland and optic nerves. As they enlarge, they typically cause visual loss, pituitary hormonal failure and headaches,” Dr. Kelly said. “Hers was a fairly typical presentation of this tumor type. The first line of treatment for a symptomatic craniopharyngioma is surgical removal. Fortunately most of these tumors can now be removed through either a nostril (the endonasal approach) or through a small incision in the eyebrow (a supra-orbital eyebrow craniotomy).”
Seeing the Light
In Odette’s case, Dr. Kelly decided the best approach would be a left supraorbital eyebrow craniotomy. This type of minimally invasive keyhole surgery differs from traditional larger craniotomies, during which a long scalp incision is placed behind the hairline and a large scalp and muscle flap is elevated to access the frontal and temporal bones.
“The eyebrow craniotomy is a relatively newer minimally invasive approach to many brain and skull base tumors in this area including craniopharyngiomas and meningiomas,” Dr. Kelly said. “With this approach, we make a short incision in the eyebrow and elevate a small area of the temporalis muscle (the chewing muscles). We then make a window in the bone directly above the eyebrow measuring about 1.5 x 2.5 cm. Through this small half moon-shaped keyhole we can access a large area around the frontal lobes including the optic nerves and pituitary gland.”
A major advantage of this approach is that it requires little to no brain retraction. The minimal scalp, muscle, bone and brain manipulation translate into a rapid and less painful recovery with a lower risk of complications and generally excellent cosmetic result. As is often the case with craniopharyngiomas, Odette’s tumor was extremely adherent and stuck to part of her optic nerves. “With tumors such as Odette’s, it is safest to leave a small remnant of tumor rather than risk worsened vision by trying to remove the entire tumor” says Dr. Kelly. Odette’s post-operative MRI shows that Dr. Kelly was able to remove 80 percent of the tumor. The remaining 20 percent was treated with focused radiation known as stereotactic radiotherapy (SRT). Now almost 5 years after surgery, Odette’s vision is much improved and the small residual tumor is getting even smaller after radiotherapy.
Worth the Trip
In the end, Odette found the journey to Dr. Kelly worth it, and she was incredibly glad she decided to fly out to be treated at Saint John’s.
“I had a great experience at Saint John’s,” Odette said. “The staff of doctors, their assistants, the nurses and the rest of the staff went above and beyond the call of duty to help in making my stay very comfortable.”
The condition and treatment of this patient may not be representative of all such cases as each situation and patient is unique.