
Be Aware of Dystonia in September
by Melita Petrossian
September is Dystonia Awareness Month!
This month, our Pacific Movement Disorders Center blog is focused on boosting awareness of dystonia. Dystonia refers to a group of distinct disorders which all share the clinical feature of involuntary abnormal muscle postures. “Dys” is Greek for abnormal, and “tonia” refers to muscle tone. In medical terms, muscle tone refers to the ability of the muscle to properly relax when at rest; it has nothing to do with muscle definition sought out by exercising. When the muscles are not properly relaxed, they may show abnormal postures, tightness or even tremor (shaking).
Types of Dystonia
Dystonia can be generalized (affecting the whole body) or focal (affecting just one body part). Almost all of us have experienced focal dystonia on brief occasions over the course of our lives – that’s what is happening when the toes and/or feet are cramping up and assuming an abnormal posture for several minutes. Another example of a focal dystonia is writer’s cramp; this also carries the name task-specific dystonia, meaning that it only comes on specific to one task, in this case writing. At all other times the tone is normal. Dystonia can also be segmental (affecting more than one body part linked by the spinal cord, such as the face and the neck, or the neck and one arm).
Dystonia can begin in childhood or adulthood. Childhood onset dystonia tends to be generalized and is more likely to have a genetic cause. Children with generalized dystonia are developmentally normal; however, if left untreated, the dystonia can cause dramatic twisting and contortions resulting in inability to run, or even walk, inability to feed oneself, inability to dress oneself, slurred speech or trouble swallowing. Typically these patients remain cognitively intact, even when they have trouble communicating due to the dystonia affecting their voice. One genetic cause of dystonia is called dopa-responsive dystonia, also known as Segawa syndrome or DYT5 dystonia. This type of dystonia typically starts in the feet but can also involve the arms and become generalized if left untreated. Luckily, as the name implies, it responds dramatically with levodopa (the precursor to dopamine), because it is caused by a biochemical lack of dopamine.
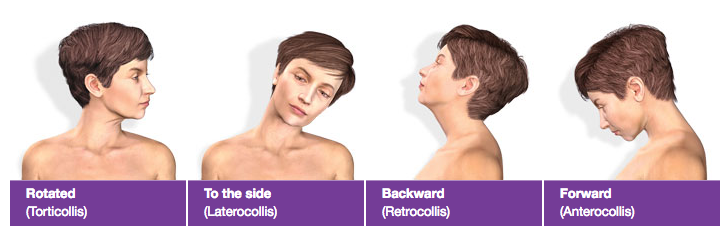
Adult-onset dystonia is more commonly focal. Cervical dystonia is one of the most common manifestations of adult-onset focal dystonia, and can manifest as neck spasm or pain, abnormal neck postures, and head tremor. Cervical dystonia is very commonly misdiagnosed initially as a musculoskeletal problem such as a pinched nerve or slipped disk. (As a clarification, cervical in this context refers to the neck, and has nothing to do with the female organ.) For more on cervical dystonia, please see my prior blog post or information from the National Spasmodic Torticollis Association (NSTA).
Other manifestations of focal dystonia include spasmodic dysphonia, which affects the muscles which control the vocal cords, causing a strangled or strained voice; blepharospasm which affects the muscles of the eyelids, causing excessive blinking and difficulty keeping the eyes open; and hemifacial spasm, which affects the muscles of one side of the face, causing twitching or tightening of muscles around the eye, cheek or mouth on one side only.
What Causes Dystonia?
The causes of dystonia are continuing to be elucidated. As mentioned above, some degree of genetic abnormality may contribute, but a majority of patients may not have any family history they are aware of. Dystonia is thought to arise from the basal ganglia (deep motor circuits of the brain) but could also have peripheral components. One theory of the onset of focal dystonia, especially when task-specific, is that there is maladaptive neural plasticity arising from the brain’s cortex. Neural plasticity refers to structural or biochemical brain changes depending on how the brain is “exercised”. For example, musicians who have very fast fine motor movements of the fingers or mouth may develop abnormal postures while playing their instruments. When not playing the instrument, their tone and neurological exam is entirely normal. Recognizing that this tends to occur more in professional musicians than in infrequent players suggests that the brain’s changes after thousands and thousands of hours of practice results in changes in motor pathways which result in abnormal movements or postures.
How Dystonia is Diagnosed
 Neurological Exam. Diagnosis of dystonia begins with a careful neurological exam focused on muscle relaxation vs. tightness, mobility or dexterity, appearance of tremor, and impact of activity / tasks such as writing, speaking, and walking. In the vast majority of cases, imaging and labs are unrevealing – that is, the MRI is normal even though the problem is arising in the brain – but such an evaluation may be required. Genetic testing can be useful in a subset of patients.
Neurological Exam. Diagnosis of dystonia begins with a careful neurological exam focused on muscle relaxation vs. tightness, mobility or dexterity, appearance of tremor, and impact of activity / tasks such as writing, speaking, and walking. In the vast majority of cases, imaging and labs are unrevealing – that is, the MRI is normal even though the problem is arising in the brain – but such an evaluation may be required. Genetic testing can be useful in a subset of patients.
Treatment Options
Botulinum Toxin
Treatment of dystonia depends on whether the dystonia is focal or generalized. Focal dystonias often respond to botulinum toxin (BoNT) injection, which is a local treatment targeting the muscles which have abnormal activity. Examples of BoNT are Botox, Xeomin, Dysport, and Myobloc. The injections are typically done every 3 months and remain effective even after years of therapy. BoNT interferes with the communication between nerve and muscle, weakening the targeted muscle. This is the same mechanism by which Botox works for wrinkles – by relaxing the muscles which cause the wrinkles. BoNT for dystonia is typically covered by insurance as it is medically necessary and not cosmetic. BoNT has been found to be effective for cervical dystonia, blepharospasm, hemifacial spasm, writer’s cramp, focal dystonia, and spasmodic dysphonia. It is also effective for certain non-dystonia conditions, but those are beyond the scope of this article. For cervical dystonia and certain focal dystonias, BoNT injection efficacy can be enhanced with physical therapy provided by neuro-certified therapists. Side effects of BoNT can include weakness of the targeted or surrounding muscle, depending on where it is injected. The side effects typically resolve within a few weeks and are never permanent.
Medication
Generalized dystonia typically requires oral medication to reduce muscle spasm. These medications include baclofen, cyclobenzaprine (Flexeril), tizanidine (Xanaflex), benzodiazepines such as clonazepam and diazepam, and anticholinergics such as trihexiphenidyl (Artane). These medications can be well tolerated by some patients but may cause sleepiness, grogginess, fatigue, weakness, blurry vision, and imbalance. Artane can also cause dry mouth, constipation, and urinary retention. These side effects resolve soon after stopping or reducing medications.
Some patients with generalized dystonia opt for the placement of a baclofen pump, instilling the medication directly into the spinal canal rather than taking it orally, resulting in fewer cognitive side effects. However, this has not been proven to be superior to other treatment options and the placement of the pump can cause issues such as infection and pump malfunction.
Deep Brain Stimulation Surgery
Patients with generalized dystonia and cervical dystonia whose symptoms have not improved with BoNT and/or oral medications may be candidates for deep brain stimulation (DBS) surgery. The deep part of the brain which contributes to the abnormal postures is typically the internal part of the globus pallidus (GPi) and by stimulating this area, DBS paradoxically reduces this abnormal motor output, causing improvement in abnormal postures and tremor. This requires the placement of electrodes into the brain and the placement of a pulse generator / battery under the skin below the clavicle, connected by wires. The entire system is internal and the electrical stimulation of the brain is painless.
Patients who are younger, with shorter duration of symptoms, and who are generally medically healthy may be good candidates for DBS. At Pacific Movement Disorders Center, we perform a multidisciplinary evaluation, including a movement disorders specialist neurologist, Dr. Melita Petrossian; restorative neurosurgeon, Dr. Jean-Philippe Langevin; DBS nurse practitioner, Giselle Tamula; and neuropsychological assessment. A specialized MRI is done to exactly localize the target. Based on this testing, a consensus opinion is rendered to determine whether the patient is a good candidate for DBS.
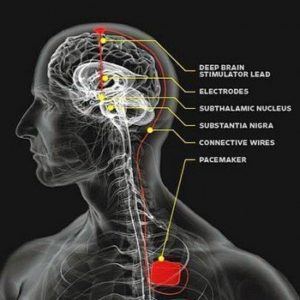
We are pleased to offer technologically advanced DBS surgery that may improve comfort and outcomes from the DBS procedure, known as frameless DBS. Because DBS electrode placement is done with the patient awake, the leads must be placed without any head movement to ensure accuracy. Traditional frame-based DBS requires the patient to lie with the head affixed to a frame, which is attached to the table. This restricts head movement and can be uncomfortable, especially for cervical dystonia patients. Frameless DBS allows for the patient’s head to move during the procedure, because the mini-frame platform is custom created for each individual patient. When the head moves, the mini-frame moves with the patient, resulting in accurate electrode placement, reduced need for pain medication during the procedure, increased comfort, and reduced procedure time. After the DBS procedure, programming of the stimulation allows for adjustments in the therapy.
Our Philosophy
Regardless of treatment plan agreed to by the patient, family and our team, the Pacific Movement Disorders Center is dedicated to providing holistic, personalized and compassionate care for all types of dystonia.
For more information or to schedule a consultation, contact us at 310-582-7433.

Dr. Melita Petrossian is Director of Pacific Movement Disorders Center and is a fellowship-trained neurologist with clinical interests and expertise in movement disorders such as Parkinson’s disease, essential tremor, dystonia, gait disorders, ataxia, myoclonus, blepharospasm, hemifacial spasm, Meige syndrome, spasticity, tics, and Tourette’s syndrome. She also specializes in Parkinson’s-related conditions such as Dementia with Lewy Bodies, progressive supranuclear palsy, multiple system atrophy, corticobasal degeneration, primary freezing of gait, and Parkinson’s disease dementia.
About the Author

Melita Petrossian
Melita Petrossian, MD, is Director of Pacific Movement Disorders Center and is a fellowship-trained neurologist with clinical interests and expertise in movement disorders such as Parkinson’s disease, essential tremor, dystonia, gait disorders, ataxia, myoclonus, blepharospasm, hemifacial spasm, Meige syndrome, spasticity, tics, and Tourette’s syndrome. She also specializes in Parkinson’s-related conditions such as Dementia with Lewy Bodies, progressive supranuclear palsy, multiple system atrophy, corticobasal degeneration, primary freezing of gait, and Parkinson’s disease dementia.
Last updated: August 2nd, 2019