
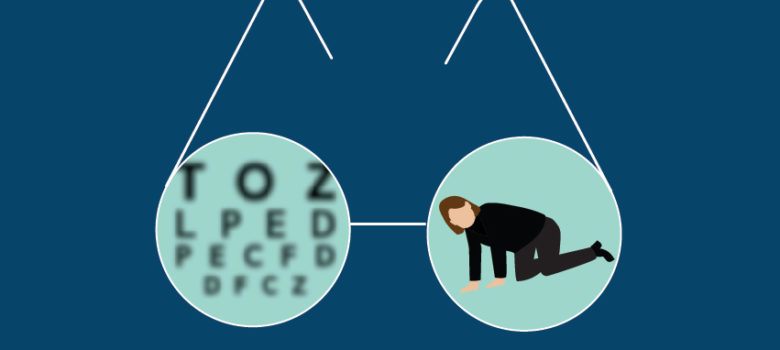
Linking eye trauma and falls among the elderly
by Guest Author
Some eye trauma hospitalization trends that a recent study tracked may not surprise physicians. However, what may be surprising is the increasing role of patient falls for many of these hospitalizations.
A study1 in JAMA Ophthalmology by focused on changes in the incidence of eye trauma hospitalizations in the U.S. between 2001 and 2014. Mustafa Iftikhar, MD, and a team of researchers led by Syed Mahmood Ali Shah, MD, examined diagnoses and procedures for each hospitalization record and used ICD-9-CM codes to identify patients with a primary or secondary diagnosis of eye trauma.
Looking at the numbers
The study found an estimated 939,608 patients with eye trauma were hospitalized in the U.S. between 2001 and 2014. Of these, 17.1% had a primary diagnosis of eye trauma, while 82.9% had it as a secondary diagnosis. Comparing 2001 to 2014, total eye trauma increased from 18.3 per 100,000 population to 22.0 per 100,000 population, respectively.
When eye trauma was the primary diagnosis, the main causes were falls (25.3%) and assault (24.7%), while eye trauma as a secondary diagnosis was associated with falls (35.2%) and auto crashes (26.6%). Among the falls, 67.3% occurred in older patients. By contrast, in children, unintentional injuries caused by objects and machinery made up the largest chunk of primary diagnosis cases (30.1%).
Among all patients, the elderly composed the largest overall age group. Most of the patients (59.3%) were male, had a lower income, were publicly insured through Medicare or Medicaid, and were from the South (36.7%).
Focusing on falls
Among the study’s findings, the connection with falls was of particular concern to the researchers. Falls continue to occur in high-risk populations, which calls for a reexamination of the existing prevention strategies. “A fall is considered a ‘never event’ in hospitals, and it’s time that we make it a never event outside the hospitals as well.” Ophthalmologists should proactively identify patients at risk for falls, Dr. Shah said.

Those at higher risk can be referred for low vision services, something that Howard R. Krauss, MD, often does. It’s also important to address fall risk with any family members present at the exam, Drs. Shah and Krauss said.
Dr. Krauss will make a note in the electronic medical record about patients who are at risk for falls, so the primary care doctor can follow up accordingly. He also sees patients at risk for falls who need further neurological assessment, particularly because he specializes in neuro-ophthalmology.
One challenge, according to Dr. Krauss, is that ophthalmologists may not always get a sense of who is at a higher risk for falls during an exam, due to the short amount of time with a patient. However, staff members may have valuable insight based on how a patient walks to and from the waiting area and exam room. Another challenge is with patients receiving certain treatments, for example, those with age-related macular degeneration who return to a practice for regular injections. Eye doctors may not always have the time to assess or ask how these patients are managing their vision loss in terms of preventing falls, Dr. Krauss said.
Ophthalmologists should take a more global view on preventing falls by working with physicians across specialties to recognize at-risk patients. Although there is a tendency nowadays to put off second eye cataract surgery, it may be that getting a second eye operation sooner rather than later could help lessen fall risk, even in borderline cases.
Beyond the falls
The study results bring attention to other eye trauma pearls that ophthalmologists can share with patients. Parents should be educated about the use of protective eyewear in children, including sports-related eye protection emphasizing the use of polycarbonate lenses.
Reference:
1. Iftikhar M, et al. Changes in the incidence of eye trauma hospitalizations in the United States from 2001 through 2014. JAMA Ophthalmol. 2019;137:48–56.
Adapted from original article in EyeWorld by Vanessa Caceres
Main image source: labblog.uofmhealth.org
For more information about neuro-ophthalmology services at the Pacific Eye, Ear & Skull Base Center at Pacific Neuroscience Institute, contact Dr. Krauss’ clinics at 310-829-8701.
For more information about Fall Prevention and Balance Treatment, contact Dr. William Buxton at the Pacific Brain Health Center at 310-582-7641.
Last updated: November 19th, 2021