I Can See Clearly Now The Tumor’s Gone
by Daniel F. Kelly
Minimally invasive keyhole surgery options for brain, skull base & pituitary tumors impacting the anterior visual pathways & eye movements.
Vision is arguably our most important sense. In fact, according to PNI neuro-ophthalmologist Howard Krauss, MD, 40% of our brain capacity is utilized for processing and acting upon visual information. As such, it is not surprising that many brain and skull base tumors are diagnosed because a patient notices deteriorating vision in one or both eyes, or they develop double vision. Preserving or restoring vision and normal eye movements is therefore one of our top goals in treating patients with such tumors.
Neuro-anatomy 101
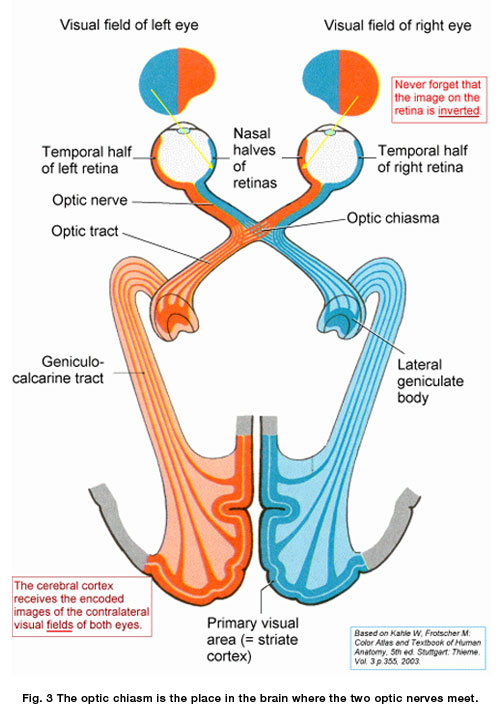
The visual pathways of the brain are amazingly complex and beautifully integrated. Starting at the retina, visual information coming into both eyes is passed along the optic nerves, optic chiasm, optic tracts back to the lateral geniculate bodies of the thalamus, then the optic radiations and ultimately to the primary visual cortex and visual association areas.
Common tumors affecting vision
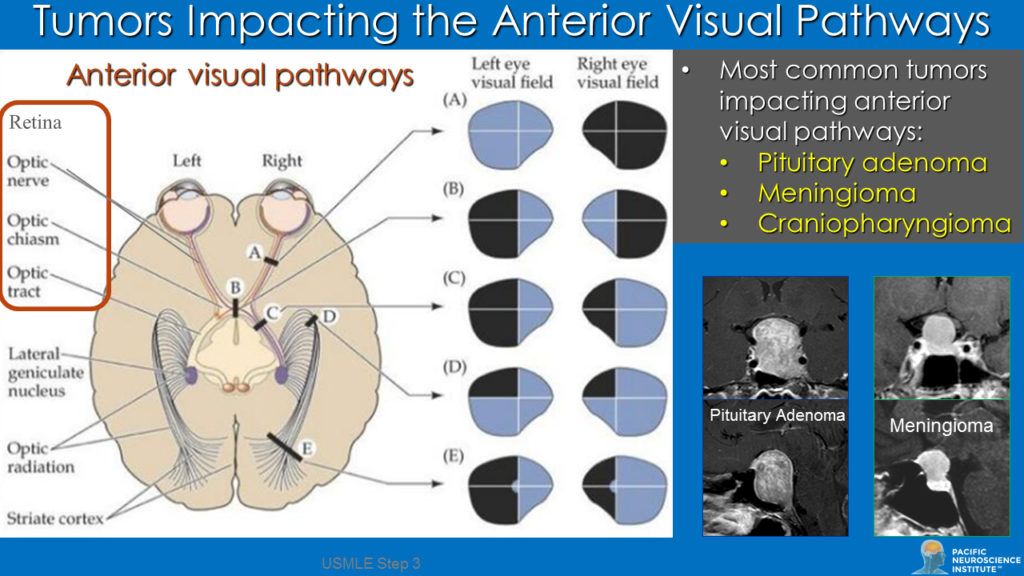
The anterior visual pathways which include the paired retinas, optic nerves, the optic chiasm and optic tracts (see diagram) are key structures of the visual system that are frequently impacted by both benign and malignant brain tumors and tumors of the skull base.
The two most common tumors impacting vision or eye movements in this region are pituitary adenomas and meningiomas; other less common tumors or cysts include craniopharyngiomas, Rathke’s cleft cysts, arachnoid cysts, chordomas, gliomas, and metastatic brain tumors. Such tumors and cysts can compress or interrupt these pathways leading to impaired central vision loss in one eye or both eyes, or visual field defects in one or both eyes.
Tumors of the skull base (particularly meningiomas and chordomas) often cause double vision (also known as diplopia) by impacting cranial nerves III, IV and/or VI as they exit the brainstem or pass through the skull base and cavernous sinus to reach the orbit. One particular entity called pituitary apoplexy (bleeding into a pituitary adenoma with swelling) can result in both acute loss of vision and/or double vision, and typically warrants urgent endonasal transsphenoidal surgery.
Making the diagnosis
Many patients with such visual or eye movement symptoms are first seen by an optometrist and eventually referred to an ophthalmologist or neuro-ophthalmologist, the latter of whom is highly specialized in diagnosing and treating patients with vision issues beginning at the optic nerves and extending back through the visual cortex of the brain, or eye movement problems beginning in the brain and extending via cranial nerves along the skull base, into the orbits to stimulate and coordinate actions of the extraocular muscles.
The diagnosis and treatment of tumors impacting vision has evolved into a highly sophisticated field with diagnostic ophthalmic testing that includes visual field testing (perimetry), optical coherence tomography of the retina to assess and measure the retinal nerve fiber layer, retinal ganglion cell layer and macula, ophthalmic fundus photography and sensorimotor testing.
These tests provide critical information objectively quantitatively documenting degree of vision loss and potential for recovery, as well as the nature and cause of double vision and which cranial nerves may be involved. The neuro-ophthalmic consultation and testing improve surgical planning, patient counseling and potential rehabilitation of visual function.
The other essential diagnostic tests are brain and skull base imaging, typically using high field (3Tesla) brain, orbital and pituitary MRIs, as well as thin-cut CT scans of the orbits and skull base. With these essential tests completed, a surgical plan can be recommended.
How we do it
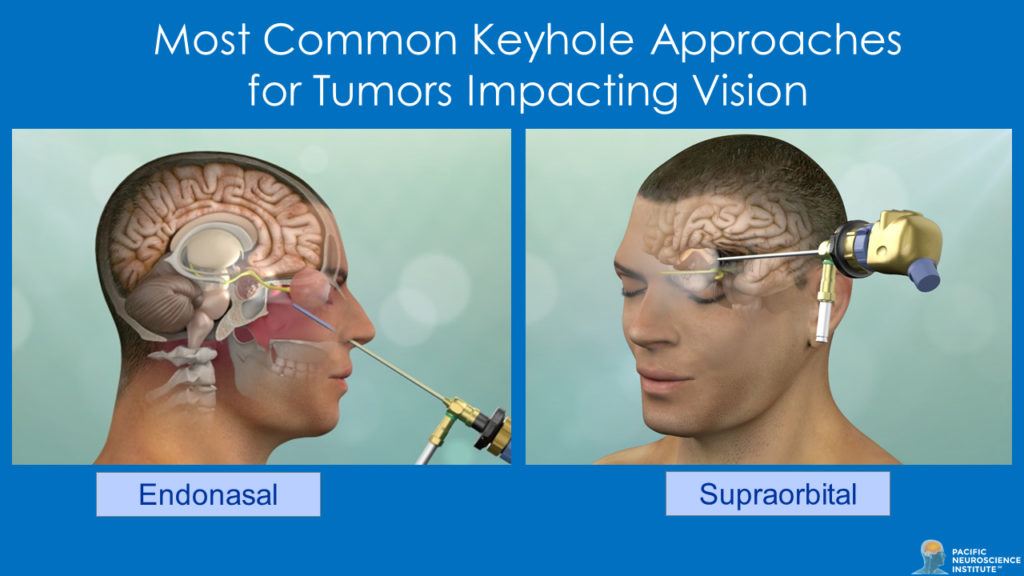
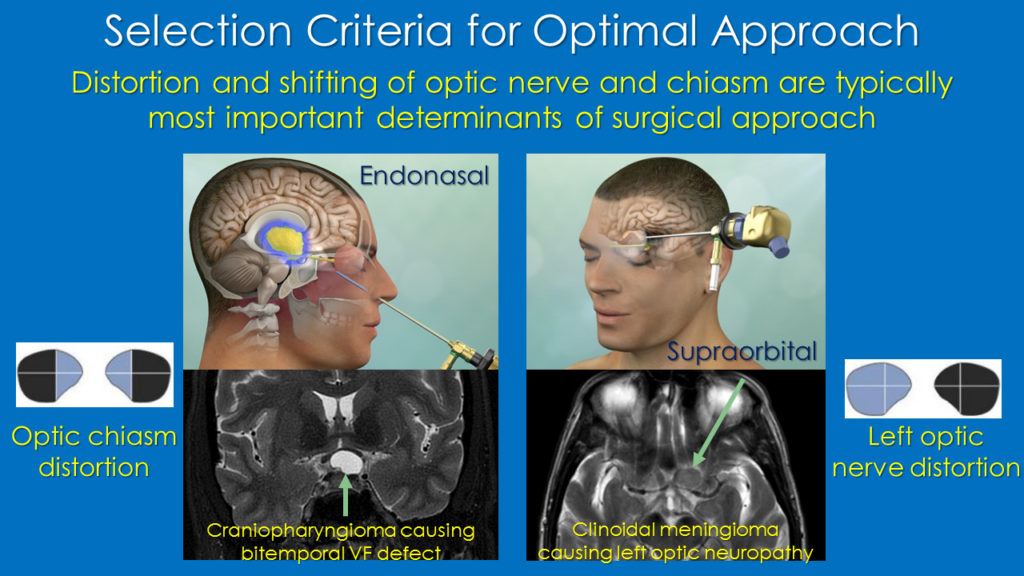
In most instances, for tumors impacting the anterior visual pathways and those causing double vision, keyhole surgery for tumor removal or maximal safe debulking is indicated. The most common approach for such tumors impacting vision is via the nose (endoscopic endonasal route), given that this route typically allows such tumors to be removed from under the optic chiasm and optic nerves with minimal or no manipulation and without retracting the brain. Alternative keyhole routes are the supraorbital craniotomy via the eyebrow, the transorbital route via an eyelid incision or the mini-pterional approach through a small incision along the side of the orbit along the temple area. The approach used is tailored to the specifics of the tumor type, location and size.
At PNI our surgical philosophy is to maximize tumor removal while minimizing risk of collateral damage and complications through experience and use of the best available technology including high-definition, endoscopy, intraoperative navigation and the Doppler probe for blood vessel localization. Most patients undergoing endonasal or keyhole craniotomy removal of a tumor impacting vision or eye movements are in the hospital for one or two nights and are back to full activities within 3 weeks after surgery.
What to expect
For our patients with vision loss from pituitary adenoma, meningioma or craniopharyngioma, vision has been restored or improved in 75-80% of cases. Full recovery may occur within a few days of surgery but in some cases, improvement occurs slowly over 6-12 months post-surgery. However, for those patients coming in with severe visual deficits, particularly long-standing and associated with atrophy of the optic nerves or chiasm, vision recovery rates are lower and less favorable.
Recovery from double vision occurs less consistently and depends upon many factors including chronicity and tumor type. Strabismus surgery, carried out by our surgeons, is usually successful in reducing the frequency of double vision for patients whose double vision persists.
Follow-up
The frequency of follow-up and need for additional therapies depends on many factors, including whether the tumor is benign or malignant and if a complete or subtotal removal is accomplished. Even patients with what appear to have complete tumor removal, may have early or late recurrences. Thus, we typically follow our patients with regular MRIs and neuro-ophthalmic evaluation and tests every 6 months for at least 2 years post-surgery and then annually for at least 10 years.
If tumor regrowth does occur, options include repeat surgery, focused radiation (or radiosurgery) and, in some instances, targeted therapies or chemotherapy, in some cases, within clinical trials.
Our publications & video library
As detailed in our publications, our PNI team has performed surgery on hundreds of patients with vision and/or eye movement deficits. These papers highlight the use of various keyhole approaches for such tumors including the endonasal and supraorbital route. Examples of these approaches are also in our keyhole surgery library.
Unique team approach under one roof
Our comprehensive team approach allows patients with brain, skull base and pituitary tumors impacting vision to be evaluated by multiple specialists under one roof in our new PNI Building in Santa Monica. For example, in one visit, our patients may see Dr. Howard Krauss (neuro-ophthalmology), Drs. Daniel Kelly or Garni Barkhoudarian (neurosurgery), Dr. Chester Griffiths (ENT), and Dr. Sarah Rettinger (endocrinology). Additional appointments may also be arranged for the same visit or on another day with our neuro-oncologists (Drs. Santosh Kesari or Jose Carrillo), or our radiation oncologists (Drs. Lisa Chaiken or Robert Wollman).
PNI team for tumors impacting vision
Neuro-Ophthalmology
Neurosurgery
ENT
Radiation Oncology
To learn more about our diagnostic workup options and minimally invasive keyhole surgery options for tumors impacting vision and eye movements, or a second opinion about a recurrent brain or pituitary tumor impacting vision, visit us at www.pacificbraintumor.org or at www.pacificpituitary.org.

Dr. Howard Krauss is Director of Ophthalmology at Pacific Eye, Ear & Skull Base Center at Pacific Neuroscience Institute, focused on skull base and orbital disease, and tumors affecting vision. He pioneered transnasal image-guided endoscopic orbital tumor surgery, for safer, less invasive and more effective approach to the management of orbital apex tumors.

Daniel F. Kelly, MD, is the Director of the Pacific Neuroscience Institute in Santa Monica, CA. Considered to be one of the top neurosurgeons in the US, Dr. Kelly is internationally recognized in the field of minimally invasive keyhole surgery for brain, pituitary and skull base tumors. He continues to focus his efforts on advancing innovative treatments for patients, providing fellowship training in minimally invasive neurosurgery, and patient education and support.
About the Author

Daniel F. Kelly
Daniel F. Kelly, MD, is the Director of the Pacific Brain Tumor and Pituitary Disorders Centers at Providence Saint John’s Health Center in Santa Monica, CA. Considered to be one of the top neurosurgeons in the U.S., Dr. Kelly is internationally recognized in the field of minimally invasive keyhole surgery for brain, pituitary and skull base tumors. He continues to focus his efforts on advancing innovative treatments for patients, providing fellowship training in minimally invasive neurosurgery, and patient education and support.
Last updated: February 15th, 2020