Cavernoma
The cerebrum – Latin for “brain” – is the coordinating center of sensation, intellectual and nervous activity.
A cavernous malformation is also called a cavernoma or a cerebral cavernous malformation (CCM), but these names are all interchangeable and refer to the same diagnosis.
Synonyms that refer to the same diagnosis include:
- Cavernoma
- Cavernous angioma
- Cavernous hemangioma
- Cavernous malformation (“Cav Mal”)
- Cerebral cavernous malformation (CCM)
What is a Cavernoma?
For simplicity we will just use the term “cavernoma.” Cavernomas are a vascular mass made up of abnormal dilated blood vessels characterized by distended blood-filled “caverns.” Vessels of a cavernoma mass have a tendency to leak and bleed because they lack the proper junctions between neighboring cells as well as the necessary structural support from smooth muscle and the stretchable material (elastin) that normally supports regular blood vessels.
Cavernomas are present in up to 0.5% of the general population, and they account for a large proportion (8-15%) of all brain and spinal vascular malformations. While more common in adults, people of all ages may be affected by them, and approximately 25% of all diagnosed cavernomas are found in children.
Cavernomas are dynamic structures, changing in size and number over time and can range in size from a few millimeters to several centimeters. The majority of cavernomas that are diagnosed occur in individuals with only a single lesion and no family history of the disease (these cases are termed “sporadic” meaning they are not caused by an inherited genetic mutation). Individuals with the familial (genetic) form of cavernomas are likely to have multiple lesions and may be more likely to experience symptoms associated with the disorder. Cavernomas are commonly associated with developmental venous anomalies (DVA) also called, venous malformations or venous angiomas. A DVA is a type of vascular malformation that, on its own, does not cause any clinical symptoms. At least 40% of sporadic cavernomas may develop within the vicinity of a DVA. The significance of DVA association with sporadic lesions is currently under investigation; perhaps this observation may suggest a difference in developmental mechanisms between sporadic and familial cavernomas.
Symptoms of a Cavernoma
In many cases, a cavernoma causes no symptoms and can go unnoticed. Leakage and bleeding from cavernomas is the underlying cause of clinical symptoms. Depending on the size and location of the cavernoma, this bleeding can cause brain damage and even in rare cases death, however, bleeding from cavernomas is often less severe than bleeding from aneurysms or AVMs because they do not contain high-pressure arterial blood flow. Symptoms of a ruptured cavernoma often come on suddenly and include a sudden, severe headache that is different from past headaches, nausea and vomiting, sensitivity to light, fainting or loss of consciousness and seizures.
Cavernoma Treatment
While a new diagnosis of brain cavernoma can produce natural anxious responses in many patients, the most important thing to remember is that you are not alone — cavernomas can occur in as many as 1 out of every 200 people – and our team of experts is here to help you understand your condition and determine an optimal, personalized treatment plan for your needs.
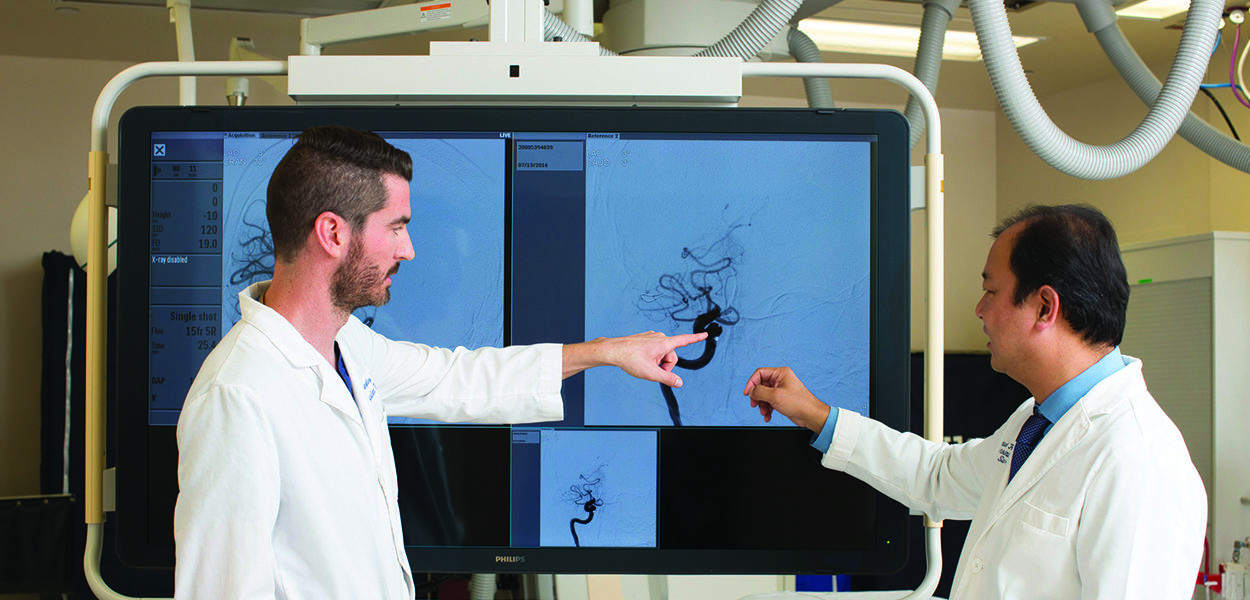
Our specialists aim to optimize medical management and minimize the need for surgery wherever possible. When refractory cavernomas do progress to require surgical removal, we offer leading-edge minimally invasive microvascular techniques, championing “keyhole” approaches. Benefits include safe corridors that minimize damage to surrounding brain tissues through smaller incisions that reduce post-operative discomfort, faster healing and recovery, and better cosmetic results. Our expert team of neurosurgeons, neuroscientists, vascular biologists and geneticists are leaders in the field of precision therapy for cavernomas, working together to offer patients multidisciplinary team-based care.
We use state-of-the-art brain imaging techniques (called diffusion tensor tractography, gradient echo and susceptibility weighted sequences) that allow for noninvasive and computational treatment planning. Most cavernomas only need to be observed with routine brain imaging, repeated over time to observe for changes in appearance, recent bleeding (“hemorrhage”) or appearance of new lesions. Medications are optimized in a patient-specific manner to treat seizures and headaches caused by cavernomas.
If however, refractory cavernomas progress despite optimal medical therapy to require safe surgical removal, our neurosurgery team is specialized in minimally-invasive microvascular techniques with “keyhole” approaches that minimize damage to surrounding brain tissues through smaller incisions that reduce post-operative discomfort and provide better cosmetic results.
Contact Us
The Pacific Stroke and Neurovascular Center’s state-of-the-art facilities are located at:
Providence Saint John’s Health Center
2125 Arizona Ave., Santa Monica, CA 90404
310-829-8319
Providence Little Company of Mary Medical Center Torrance
4201 Torrance Blvd., Suite 520, Torrance, CA 90503
424-212-5340
Providence Saint Joseph Medical Center
501 S. Buena Vista Ave., Burbank, CA 90505
818-847-6049
Providence Holy Cross Medical Center
15031 Rinaldi St, Mission Hills, CA 91345
818-847-6570

