Rathke’s Cleft Cyst
What is Rathke’s Cleft Cyst?
Deep within the recesses of the pituitary gland lies Rathke’s Cleft Cyst, a remarkable anomaly originating from embryonic tissue remnants. Formed during the early stages of development, the cyst emerges from the Rathke’s pouch—a critical structure responsible for the formation of the pituitary gland. Rathke’s Cleft Cyst are fluid-filled masses arising within or above the pituitary gland & may cause loss of hormonal function, visual loss and/or headaches. nIt’s important to note that RCC is classified as a noncancerous (benign) developmental cyst, making it distinct from other pituitary tumors. While the cyst’s presence may not be immediately apparent, it can significantly impact hormone production and lead to various pituitary gland dysfunctions.
Symptoms of Rathke’s Cleft Cysts
Unraveling the mysteries of Rathke’s Cleft Cyst requires awareness of its associated symptoms. Individuals with RCC may experience a range of manifestations, including debilitating headaches, changes in vision, disruptions in hormonal balance, and pituitary gland dysfunction. Prompt diagnosis is crucial, involving a comprehensive approach that combines meticulous physical examinations, advanced imaging studies such as magnetic resonance imaging (MRI) and computed tomography (CT) scans, as well as hormone level tests. At Pacific Neuroscience Institute, our multidisciplinary team of neurosurgeons, endocrinologists, and specialists collaborate to provide a thorough evaluation, ensuring accurate diagnosis and tailored treatment plans.
Diagnosis & Treatment
Over half of all Rathke’s Cleft Cysts seen in our practice are incidental findings, cause no symptoms or hormonal problems, and require no treatment. However, for patients with a symptomatic (and typically larger) Rathke’s cleft cyst, endoscopic endonasal surgical removal (via the nose) is the treatment of choice. Fortunately, there have been major technical advances in this surgical approach over the last two decades, including use of high-definition endoscopy, surgical navigation techniques and more effective skull base closure methods.
At Pacific Pituitary Disorders Program, we have one of the world’s largest experiences in transsphenoidal endoscopic endonasal surgery. By incorporating cutting edge technology and instrumentation with proven surgical experience of over 2,000 endonasal surgeries, we make Rathke’s Cleft Cyst surgery safer, less invasive and more effective. Dr. Kelly and his team also have a large surgical experience treating patients who have had prior surgery for a RCC.
Overview
Rathke’s Cleft Cysts are not true tumors or neoplasms; instead they are benign cysts.
Rathke’s Pouch
Rathke’s pouch forms as part of normal development and eventually forms the anterior lobe, pars intermedia and pars tuberalis, of the Pituitary Gland. This pouch normally closes in fetal development, but a remnant often persists as a cleft that lies between the anterior and posterior lobes of the pituitary gland.
Rathke’s Cleft Cyst Symptoms
Occasionally, this remnant enlarges to form a cyst. Rathke’s Cleft Cysts can cause:
- Pituitary failure
- Headaches
- In some instances, vision loss
Diagnosis
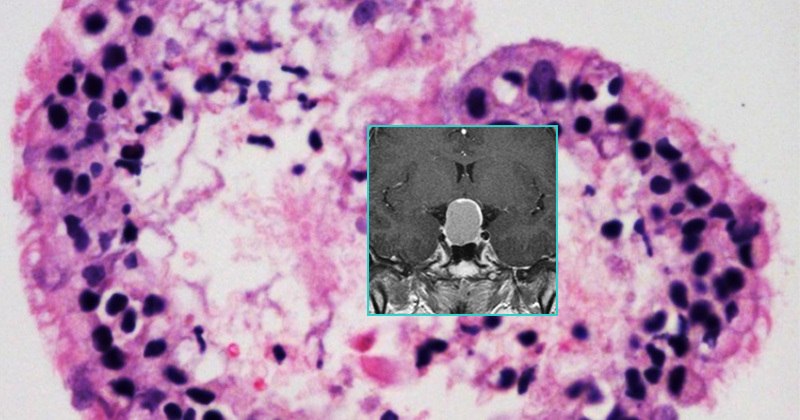
Symptomatic Rathke’s Cleft Cysts are relatively common pituitary lesions, accounting for 5-10% of surgically removed pituitary masses. Rathke Cleft Cysts can be seen at any age, although most are identified in adults. However, many intrasellar Rathke’s Cleft Cysts that are within the pituitary gland may be quite small, are usually asymptomatic and are found incidentally at autopsy or on a magnetic resonance imaging (MRI) scan.
These smaller Rathke Cleft Cysts rarely need treatment and can be simply “followed” with regular MRIs every year or so. However, larger RCCs (typically > 1 cm in maximal diameter) may cause visual disturbances, symptoms of Pituitary Dysfunction, and headaches and do often require surgical removal.
The typical means of visualizing a Rathke’s Cleft Cysts is with an MRI or a computer tomography (CT) scan of the pituitary region performed without and with contrast. A complete pituitary hormonal blood evaluation should also be performed.
Other possible diagnoses to consider when a cystic mass is seen in the area of the pituitary include a cystic pituitary adenoma, craniopharyngioma or arachnoid cyst.
Treatment
Rathke’s Cleft Cyst surgery is the standard treatment for symptomatic RCCs causing pituitary failure, headache or visual loss.
Typically, this requires surgical removal through an Endoscopic Endonasal Surgery. The goal of surgery is to completely remove the cyst contents while improving or preserving pituitary function vision and alleviating headache and visual loss if present. Attempts to remove the cyst lining should be avoided because this can result in pituitary gland damage. A complete removal of Rathke’s Cleft Cysts is possible in 80-95% of cases although they can recur at a rate of 5 – 15% over 5 to 10 years.
Endoscopic Endonasal Video
Is Rathke cleft cyst dangerous?
Usually not – in some cases it can grow significantly and cause vision loss. In rare cases, in can rupture or bleed which can be a surgical emergency.
Is Rathke cleft cyst a brain tumor?
No, Rathke’s cleft cyst is not a brain tumor.
Can a Rathke’s cleft cyst grow?
Yes, typically growth is 1-2 mm / year.
Is Rathke cleft cyst hereditary?
No, Rathke’s cleft cyst is not hereditary.
How long does surgery to remove Rathke cleft cyst take?
It depends on the type, but often 2-3 hours.
What is recovery from the surgery like?
Most patients are upright, eating breakfast the next morning and likely able to leave the hospital after one evening.
Once removed, will Rathke’s cleft cyst come back?
There is a small chance (1%/year) that the cyst could come back – requiring monitoring with serial MRIs.
Doctors And Specialists Who Treat Rathke’s Cleft Cysts
At the Pacific Pituitary Disorder Center our doctors and specialist have years of experience treating Rathke’s cleft cyst and other pituitary disorders that are complex in their diagnosis and treatment & warrant a team approach of experienced specialists to achieve optimal outcomes. From diagnosis to treatment, as well as education and support, we are here for you.