
The Resilient Pituitary Gland
by Garni Barkhoudarian
The pituitary gland is considered to be the “master endocrine gland”. It is a pea-sized structure located at the base of the brain, important in controlling growth and development and the functioning of the other endocrine glands. Hormones secreted from the pituitary gland help control growth, blood pressure, certain functions of the sex organs, thyroid glands and metabolism as well as some aspects of pregnancy, childbirth, nursing, water/salt concentration and the kidneys, temperature regulation and pain relief.
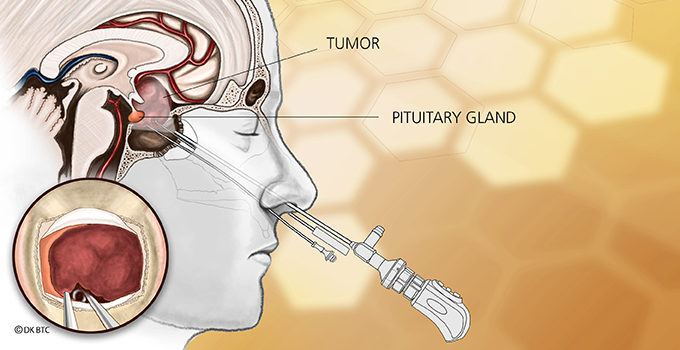
Pituitary tumors are the third most common intracranial tumor. For the majority of symptomatic pituitary adenomas, Rathke’s Cleft Cysts (RCCs) and craniopharyngiomas, transsphenoidal surgical removal (via the nose) performing Endonasal Endoscopic Surgery is the treatment of choice.
Given their location, tumors in and around the Pituitary Gland can cause significant health problems and disability including abnormal pituitary hormone over-production (e.g., acromegaly – excess growth hormone; Cushing Disease – excess adrenocorticotropic hormone; prolactinoma – excess prolactin; thyrotropinoma – excess thyroid stimulating hormone), hormonal underproduction (hypopituitarism), loss of vision, headaches and bleeding.
For this reason, operating on pituitary tumors can be challenging as presenting symptoms can be quite diverse. A patient with headaches and vision loss has different goals than a patient with Cushing Disease.
Nevertheless, the preservation of pituitary gland function is preferred, despite readily available medications to replace most of its hormones. Only a patient on life-long hormone replacement for cortisol or vasopressin (anti-diuretic hormone – ADH) can tell you the challenges of stress hormone dosing and maintenance of fluid balance. Women attempting to conceive have additional challenges when their glands are not working, often requiring the assistance of fertility specialists to prime their ovaries. So, whenever there is a concern about damaging the pituitary gland during surgery, we consider the reason seriously and think twice about the overall goals.
A primary example of this is when surgeons need to deliberately incise or resect the normal pituitary gland in order to reach pituitary tumors behind the gland. The purported concept for such a maneuver is to prevent excessive traction on the pituitary gland – and in turn, the pituitary stalk and hypothalamus. However, this theory had never been supported by data until our recent publication in the journal Pituitary. By analyzing our patients who had surgery for common pituitary tumors (adenomas) and cysts (372 patients over 4 years), we found that there was no significant increase in pituitary dysfunction and the rate of temporary dysfunction with ADH secretion actually decreased. Interestingly, patients who underwent hemihypophysectomies (removing half the normal gland for Cushing Disease) had no new pituitary hormone dysfunction at all.
Though we utilize technology to improve our ability to safely remove pituitary tumors using the endoscopic endonasal approach with high definition visualization, neuronavigation and Doppler ultrasonography, the technical goals of surgery remain in-line with this philosophy.
About the Author

Garni Barkhoudarian
Dr. Garni Barkhoudarian is an expert neurosurgeon and director of the Facial Pain and Adult Hydrocephalus Centers, and Co-director of the Pituitary Disorders Center at Pacific Neuroscience Institute. His philosophy for virtually all intracranial procedures is to apply the keyhole concept of minimizing disturbance to the brain and its supporting structures.
Last updated: May 3rd, 2022